Background: Pulmonary embolism (PE), refers to obstruction of the pulmonary artery or one of its branches by material (thrombus, tumor, air or fat) that originated elsewhere in the body.Wells criteria must be part of the clinical assessment for PE. With these criteria, we can classify patients as high probability (>6 pts), moderate (2 to 6 pts), or low (<2 pts) for PE. Pulmonary embolism rule-out criteria (PERC) rule, is used for patients previously classified as low probability for PE as per Wells Criteria, and includes age 95%, no hemoptysis, no estrogen use, no prior DVT or PE, no unilateral swelling, no surgery/trauma requiring hospitalization in the previous 4 weeks. Patients that fulfill all criteria, have a low likelihood of PE and no further testing is recommended. By the other hand, the rest of the patients may need further testing (i.e. D dimer).It is unknown in our institution how many patients as per Wells criteria were low, intermediate or high probability for Pulmonary embolism in the ED, and furthermore in the low risk group, how many patients meet all 8 PERC rule criteria in order to avoid the use of CT pulmonary angiogram as a diagnostic method.
Methods: Prospective study of the patients that underwent CTPA to rule out PE, in the ED in Trinitas Regional Medical Center, Elizabeth-New Jersey from January 2019 to June 2019. Patients were classified as per Wells Criteria in low, intermediate and high risk for PE. In the low risk group, PERC rule was applied to assess which patients needed further work up for PE and who did not, however this did not preclude to order CTPA if considered by ED physicians. Age-adjusted D-dimer was used for low and intermediate risk patients. Negative predictive value of PERC rule/age-adjusted D-dimer was calculated as well.
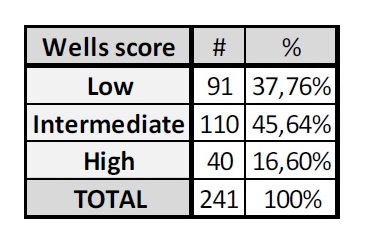
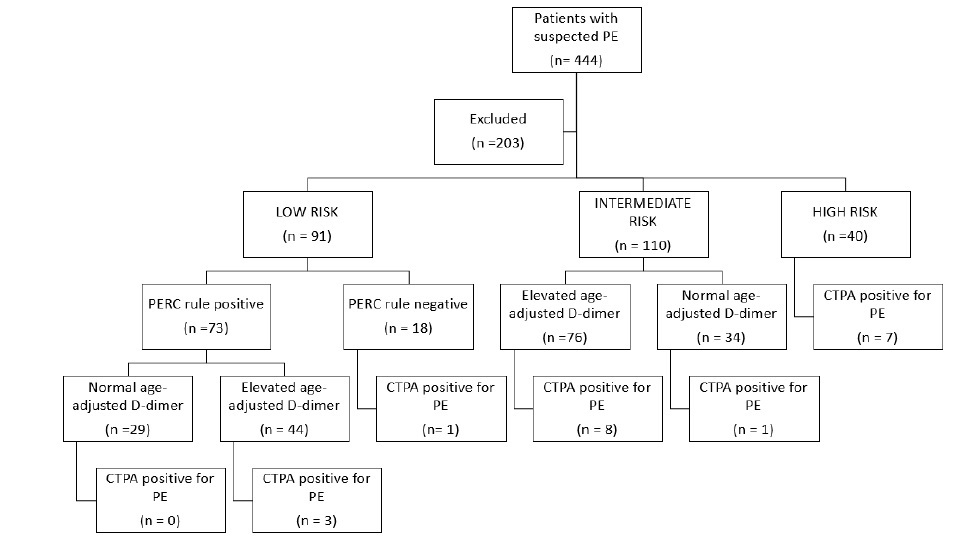
Results: A total of 444 patients were analyzed. Of these, 45.7% (N = 203) were excluded due to incomplete documentation. Average age was 50.12 + 17.78 years, with a female predominance of 59.75% (n=144).Ninety one were considered low risk, of which, 80.22% (n=73) were PERC rule positive (+).From the PERC rule negative (-) patients, only 1 had PE. For PERC +, age adjusted D-Dimer was applied.From those, 60.27 % (n=44) had elevated age adjusted D- Dimer (> 250 ng/ml).CTPA in this group showed PE in 6.82% (n=3).Together, PERC – and PERC + with a normal age-adjusted D-dimer, only 2.13% (n = 1) had PE in CTPA.Negative Predictive Value (NPV) was 97.87% (95% CI, 89.28% to 99.61%).In patients PERC – and PERC + with normal age-adjusted D-dimer, CTPA could be avoided in 51.65%. On the other hand, one hundred ten patients were classified as intermediate risk, with a 69.09% (n=76) having an elevated age-adjusted D- Dimer.CTPA was positive for PE in 10.53% (n=8) in elevated age-adjusted D-dimer patients vs 2.94% (n=1) in normal age-adjusted D-dimer.NPV was 97.06% (95% CI, 83.58% to 99.53%).In the intermediate risk group, patients with a normal age-adjusted D-dimer, CTPA could be avoided in 30.91% of the cases.
Conclusions: Applying clinical decision rules are effective means of reducing costly diagnostics. The PERC Rule and Wells Criteria are validated clinical decision rules that decrease radiation exposure, improve ED through put and mitigate advanced imaging consumption. It is important to educate the clinical staff at Community hospitals on the nuances of D-dimer assays so that the proper clinical application can be applied.