Background:
Acute pancreatitis is among the most common and costly reasons for hospitalization in the United States. While bowel rest, pain control, and intravenous fluids are the cornerstone of treatment, recent evidence suggests that early rather than delayed feeding may be beneficial. Guidelines, however, continue to recommend waiting for clinical improvement before feeding. We thus performed a systematic review and meta-analysis to evaluate the effect of early versus late enteral feeding on duration of hospitalization and complications in patients with acute pancreatitis.
Methods:
We searched for randomized controlled trials in the following databases: Medline via Ovid (1950-present), Embase (1946-present), Cochrane CENTRAL (1948-present), the CINAHL (1960-present), and Web of Science via Scopus. Two authors independently reviewed and abstracted studies if they: (a) included adults hospitalized with acute pancreatitis and (b) compared early (within 48 hours) to delayed enteral (oral or nasoenteric) feeding. Our primary outcome of interest was length of hospital stay. Secondary outcomes included mortality, readmissions, feeding intolerance, complications of pancreatitis and gastrointestinal symptoms (e.g., nausea, vomiting). Risk of bias was assessed using the Cochrane Collaboration tool. Mean differences in hospital length of stay and cumulative risk differences for secondary outcomes were pooled using the Hartung-Knapp-Sidik-Jonkman random effects method. Subgroup analysis was performed to determine whether severity of illness, geographic region, study quality, or route of nutrition affected the association with length of stay. Sensitivity analyses included fitting fixed effects models.
Results:
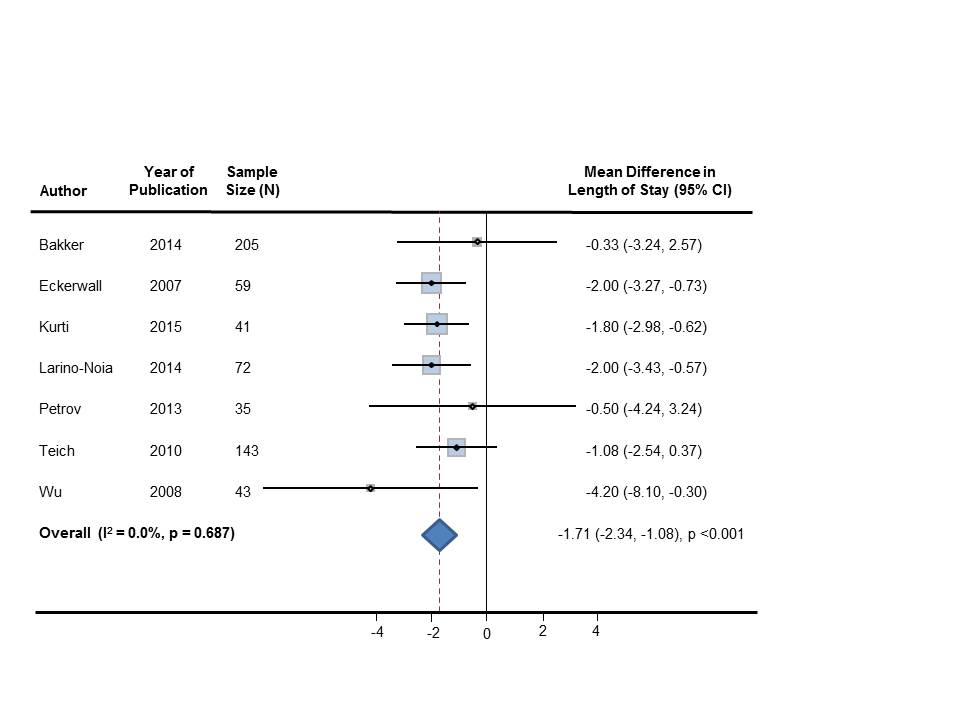
Of 991 citations identified, 7 studies with 598 patients met eligibility criteria. Early feeding was associated with a 1.71 day reduction in length of hospital stay (95% CI: -2.34 days, -1.08 days; p<0.001, τ2=0.0; I2=0%). Length of stay was less in early (vs delayed) feeding in both nasoenteric and oral feeding subgroups (p=0.04, p=0.03 respectively). Hospital readmission occurred in 6.4% of patients with early and 10.3% of patients with late feeding (p=0.16). Feeding intolerance developed in 6.3% of the early compared to 23.6% in the late group (p=0.15). Rates of death, nausea, vomiting, necrotizing pancreatitis, and recurrent abdominal pain were similar across both groups.
Conclusions:
Early initiation of feeding in acute pancreatitis is associated with reduced hospital stay and does not result in increased rates of readmission, complications or death. Greater adoption of early feeding in acute pancreatitis may produce substantial cost savings for hospitals in the United States.