Background: The In-hospital Mortality for Pulmonary embolism using Claims daTa (IMPACT) rule has been validated in a number of commercial and all-payer claims databases; classifying pulmonary embolism (PE) patients into low- and higher-risk in-hospital all-cause mortality categories with a sensitivity of 87% and specificity of 47%. We sought to directly compare the accuracy of IMPACT and three clinical prediction rules for prognosticating in-hospital mortality.
Methods: We retrospectively identified consecutive adult patients presenting to our institution with acute, objectively-confirmed PE between 11/21/2010 and 5/12/2015. Patients undergoing thrombolysis or embolectomy within 48-hours of presentation were excluded. The accuracy of the IMPACT (estimated in-hospital mortality=1/[1+exp[-x]; where x= -5.833+[0.026*continuous age] +[0.402*myocardial infarction]+[0.368*chronic lung disease]+[0.464*stroke]+[0.638*prior major bleeding]+[0.298*atrial fibrillation]+[1.061*cognitive impairment]+[0.554*heart failure]+[0.364*renal failure]+[0.484*liver disease]+[0.523*coagulopathy]+[1.068*cancer]; low-risk defined an estimated mortality ≤1.5%), PE Severity Index (PESI), simplified PESI (sPESI) and Hestia rules for prognosticating in-hospital all-cause mortality were compared.
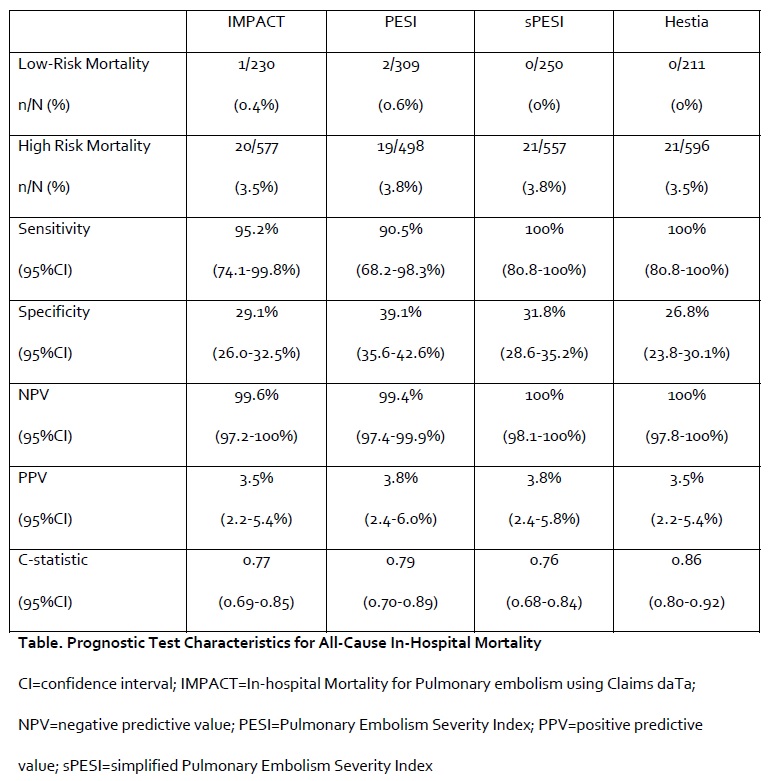
Results: In total, 807 PE patients were included and 21 (2.6%) died prior to discharge. IMPACT, PESI, sPESI and Hestia classified 28.5%, 38.3%, 31.0% and 26.1% of PE patients, respectively, as low-risk for in-hospital mortality. The case fatality rate among these low-risk patients across the different rules was low (0 to 0.6%) corresponding to NPVs for in-hospital mortality for all rules being ≥99.4% (Table). IMPACT had a sensitivity of 95% for predicting in-hospital mortality; while the sensitivities of the 3 other rules ranged from 91 (PESI) to 100% (sPESI and Hestia). The c-statistics for the rules ranged from 0.76 (sPESI) to 0.86 (Hestia).
Conclusions: IMPACT identified low-risk PE patients with similar accuracy as commonly used prediction rules. While not designed for prospective clinical-decision making, IMPACT appears useful for identification of low-risk PE patient in retrospective claims-based studies.