Case Presentation: A 2-year-old girl with a past medical history of hypertension and anterior mediastinal mass of unclear etiology presents to the ED with acute bruising. 2 months prior, she was admitted to PICU for fever and lethargy, AKI, hyperuricemia and electrolyte abnormalities concerning for tumor lysis syndrome (TLS), and was found to have a mediastinal mass on chest CT scan. With extensive fluid rehydration, her AKI and electrolyte abnormalities improved. After discharge, outpatient work up included a bone marrow biopsy that was negative for malignancy, and a cardiac MRI was scheduled.
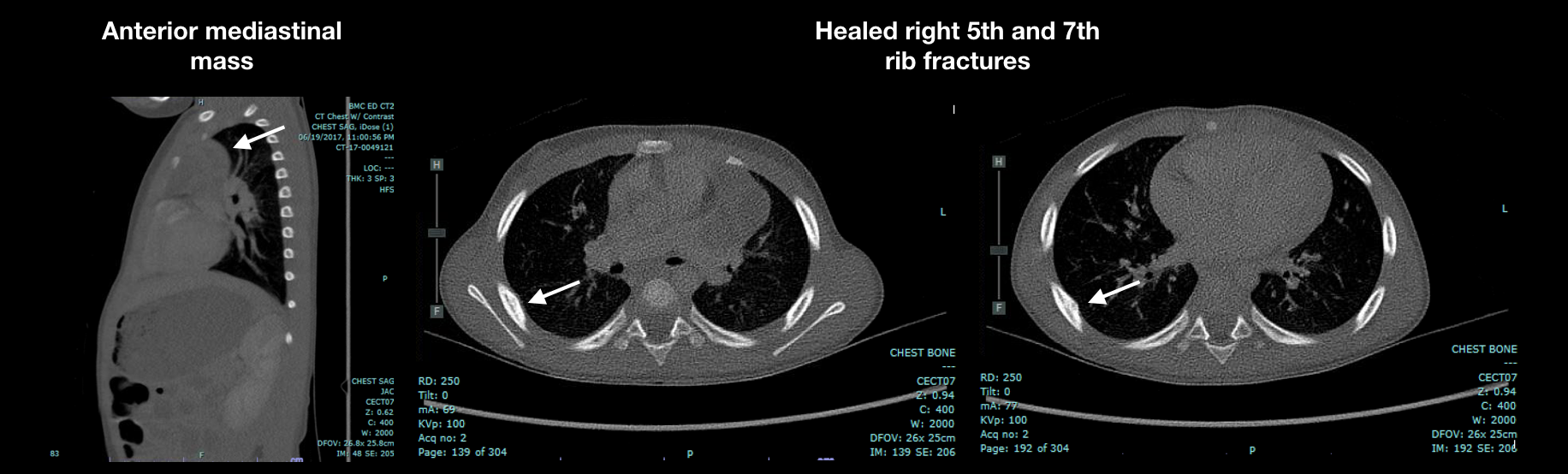
Prior to this ED visit, she awoke with bruising over her right ear and anterior chest. Her vital signs show her to be afebrile, normotensive, tachycardic to 124 bpm, and tachypneic to 30 breaths/min. Physical exam reveals her to be alert and appropriate, with visible bitemporal circular bruises; bruises on right ear pinna and posterior auricular area; and 3 circular anterior chest bruises at clavicular level. Lab findings include WBC 9.3 K/mm3, Hgb 9.3 g/dL (MCV 68.9 fL) PT 11.9s (INR 1.1), PTT 24.1s, ESR 22 mm/hr, platelet 423 K/mm3, lipase U/L, uric acid 6.5 mg/dL, phos 5.3 mg/dL, creatinine 0.3 mg/dL, AST 965 U/L, ALT 1302 U/L, uric acid 6.5 mg/dL, LDH U/L 994, alkaline phosphate 859 IU/L. Chest x-ray shows new smooth bony contour convexities at the inferolateral aspect of the right 5th and 7th ribs. Repeat chest CT scan reveals no changes in the mass, but healed right 5th and 7th rib fractures are identified on posterior thorax. Non-accidental trauma (NAT) is diagnosed and custody of child is obtained by the DCF. Ultimately she is referred to a quaternary care children’s hospital where biopsy reveals multiloculated thymic epithelial cyst, uninvolved thymus gland, and no evidence of malignancy. The etiology of the spontaneous TLS remains unclear.
Discussion: Children undergoing evaluation and treatment for complex medical illnesses are at increased risk for child abuse and neglect. Increased needs for care and additional stressors on parents and caregivers lead to increased risk. Findings of NAT in this population frequently go unnoticed due to difficulties differentiating them from other abnormalities associated with concurrent medical illnesses. Limited mobility, spasticity, and being nonverbal can also hinder the diagnosis of NAT in this population. Bruising pattern suspicious for NAT always requires further workup regardless of underlying medical illness even if associated with bruising. Bruises over ears and trunk have higher odds ratio of having NAT. Thymic cysts account for 3-5% of mediastinal masses, and multilocular thymic cysts are thought to be acquired lesions associated with inflammatory conditions and/or malignant tumors. Associated conditions can include acquired immunodeficiency syndrome, Sjogren syndrome, systemic lupus erythematosus, myasthenia gravis, and follicular lymphoid hyperplasia of the thymus.
Conclusions: Health care providers caring for children with acute and chronic medical illnesses should have a higher clinical suspicion for NAT. Manifestations of NAT can be confused for those of underlying illnesses. Additional support and resources should be provided to reduce the risk of NAT in this population.