Background:
The Centers for Medicare and Medicaid Services (CMS) recently changed observation and inpatient status determination from a decision based on clinical criteria to one based on time spent under care. Effective October 1, 2013, encounters ≥ 2 midnights should be inpatient, and those < 2 midnights, with rare exceptions, should be observation. It is not known how this rule change has actually impacted clinical practice.
Methods:
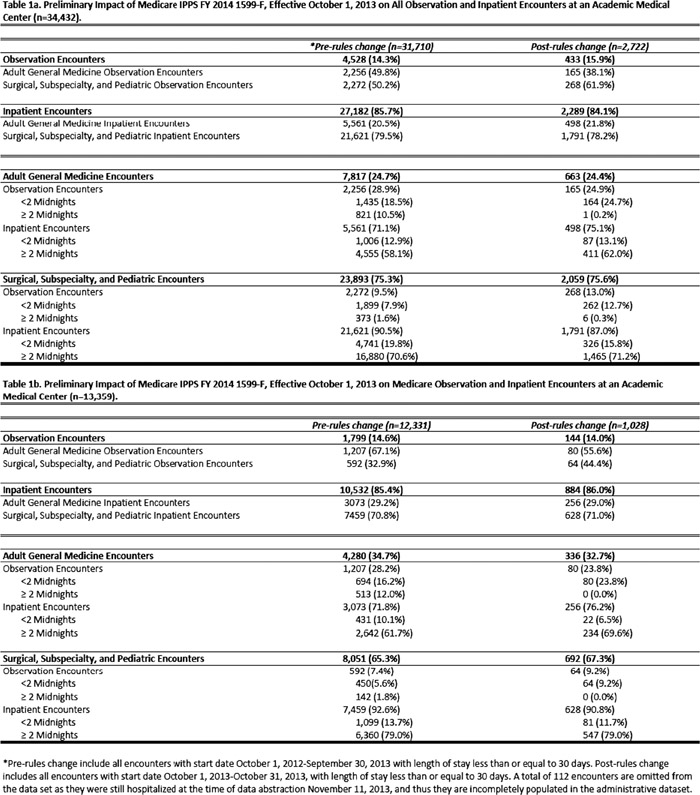
All encounters at University of Wisconsin Hospital and Clinics with start dates between 10/1/2012‐10/31/2013, and length of stay (LOS) less ≤ 30 days were included in this analysis, with intent to include encounters through 12/31/2013 in the final presentation. On the day of data abstraction (11/11/2013), 112 encounters were still active (not discharged), and were excluded because the administrative data set variables are not fully populated until after discharge.
Pre‐rules change encounters are those with a start date of 10/1/2012‐9/30/2013; post‐rules change with start dates 10/1/2013‐10/31/2013. Observation or inpatient status, LOS <2 midnights or ≥ 2 midnights, insurance, and discharging service were recorded for all encounters. Adult General Medicine encounters were those discharged from one of the hospital’s general medicine or adult family medicine services. Skilled nursing facility discharges, cost, reimbursement and ICD‐9 codes will be presented with the completed data set.
Results:
There were 34,432 encounters over the 13 month period, 38.8% (13,359/34,432) of which had Medicare as the primary payor. Adult General Medicine encounters made up one‐quarter (24.6%) of overall encounters, and about one‐third of Medicare encounters (34.6%). The overall percentage of observation encounters increased after the rules change (14.3% to 15.9%), with a slight decrease in the Medicare‐only population (14.6% to 14.0%) (Figure). Long (≥ 2 midnight) observation stays were essentially eliminated post‐rules change. The overall proportion of observation services delivered on Adult General Medicine services decreased post‐rules change (49.8% to 38.1%), with a proportionate increase in non‐medicine observation encounters (50.2% to 61.9%). Despite the decrease in Adult General Medicine observation encounters, nearly one in four Adult General Medicine encounters were still observation post‐rules change (28.9% to 24.9% for all; 28.2% to 23.8% for Medicare‐only). Notably, the proportion of surgical, subspecialty and pediatrics observation encounters increased after the rules change overall (9.5% to 13.0%) and for Medicare‐only (7.4% to 9.2%).
Conclusions:
Application of the “rules change” to all populations at our hospital resulted in an overall increase in observation encounters, yet a decrease in Medicare observation encounters. This may reflect a higher proportion of Adult General Medicine patients in the Medicare population. We also found that long observation encounters have been virtually eliminated at our institution. Despite these findings, the new rule has not had a meaningful impact on our very high observation rate. One in 7 of all hospital encounters, and 1 in 4 general medicine encounters remain observation after the rules change. The increased observation rate on surgical services, which may reflect conversion of short inpatient stays to observation, may have significant longitudinal financial implications for patients and institutions. The addition of cost and reimbursement figures to this data will illustrate the financial impact of this rule.