Background: Early and sustained mobilization of patients throughout admission is a goal we all strive to achieve. Inpatient immobility leads to the development of medical complications such as pressure ulcers, acute venous thrombosis, nosocomial infections, decreased muscle mass, and overall functional decline. Additionally, patients become deconditioned from their baseline and require potentially preventable additional services at home or placement at a sub-acute rehabilitation facility. Unfortunately, a common practice is to avoid patient mobilization prior to ordering a physical therapy (PT) consultation due to a fear of patient injury or fall. However, this practice leads to a reduction in patient mobilization, an increase in unnecessary bedrest orders and a strain on the inpatient physical therapy team.
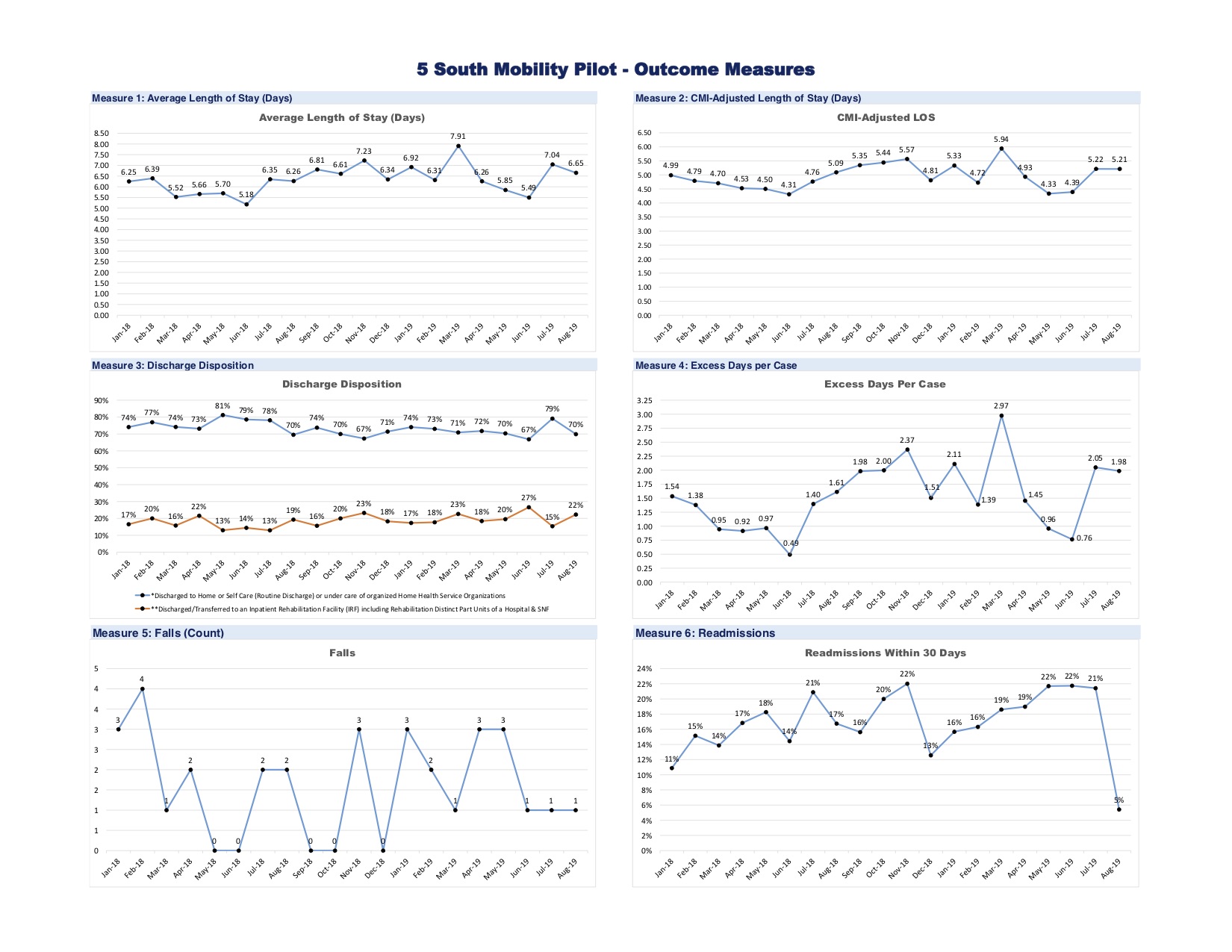
Purpose: At our large urban academic tertiary care institution, we utilized unit staff to promote early and continued mobilization of every patient admitted to the general medicine floor. Two process measures included: 1) compliance with the admission functional assessment and 2) twice daily mobilization. The number of falls and functional status were monitored daily. Outcome measures included length of stay and discharge disposition.
Description: Our innovation was piloted on a 37-bed general medicine unit. Over a month, floor nurses and staff were educated on the benefits of early mobilization and were oriented to the assessment protocol to be used on newly admitted patients. The initial patient assessment included characterizing the patient’s baseline mobility prior to getting ill. Patients were deemed bed bound, bed to chair bound, ambulatory with assist, or independent. A standardized functional assessment tool (Activity Measure for Post-Acute Care “AM-PAC”) 6 Clicks Score was used to measure the patient’s mobility. AM-PAC 6 Clicks is a questionnaire with a total score of 5 to 24, with 24 being fully functional and independent and 5 being bed bound and fully dependent. The patient would be walked by staff once every 12-hour shift to their highest level of ability. The Johns Hopkins Highest Level of Mobility Scale was used to determine the level of assistance the patient would need. On discharge, another AM-PAC 6 Clicks score would be assessed to determine if there was any change. Hospitalists and house staff played an integral role by incorporating mobilization as part of their care plan and interdisciplinary rounds.
Conclusions: Over a 6-month timeframe, we achieved close to 100% compliance with the intervention. The number of falls decreased from 3 per month to 1 per month. The AM-PAC 6 Clicks score on discharge revealed 6% of patients had functionally declined versus 15% on another comparable medicine floor that did not implement early mobilization. Length of stay and discharge disposition remain stable but it is too early to measure any appreciable change. We emphasize the importance of assessing a patient’s the functional status prior to hospitalization. Patients are often misconstrued as too sick or too old to ambulate, which leads to the lack of mobility and possible adverse outcomes. As healthcare providers, we not only aim to have our patients feel better but to get better.