Background: The economic burden of illness for patients with major depressive disorder (MDD) with suicidal ideation (SI) and suicide attempt (SA) can be attributed to the intensive level of care required, as these patients are frequently evaluated in the emergency department (ED) and admitted to the hospital. This study evaluated this burden of hospitalized patients with MDD and SI or SA (SI/SA).
Methods: Patients ≥18 years of age diagnosed with MDD and SI/SA during an ED visit or inpatient admission were identified from the Premier Hospital database between 1/1/2014 and 6/30/2017. Patients were required to have either MDD as the primary and SI/SA as the secondary hospital discharge diagnosis, or SI/SA as the primary and MDD as the secondary hospital discharge diagnosis. The earliest admission or ED visit was defined as the index event. Patients were excluded if they had diagnoses of psychosis, schizophrenia, bipolar disorder, mania, or dementia. Patient demographics and clinical characteristics, length of stay (LOS), and hospital costs during the index event were evaluated for the overall population, by crisis setting (ED, inpatient) and inpatient LOS (categorized as short: 1-3 days; medium: 4-5 days; long: ≥6 days). ANOVA and Chi-square tests were used for the comparison of continuous and categorical measurements among patient cohorts.
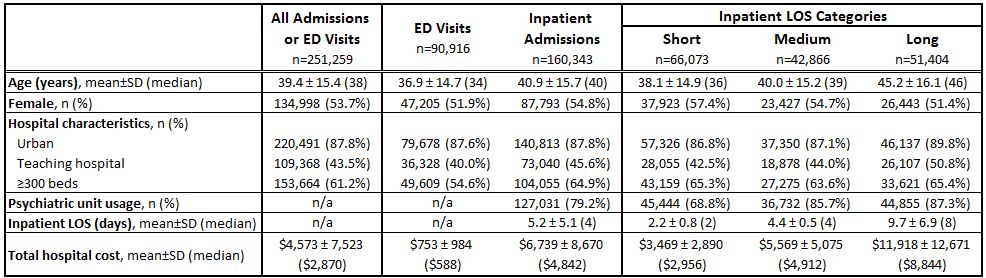
Results: Of the 251,259 patients identified, 90,916 (36.2%) were treated in the ED (mean age: 36.9; 51.9% female) and 160,343 (63.8%) were admitted to the inpatient setting (mean age: 40.9; 54.8% female; mean LOS: 5.2 days) (Table). Within the ED and inpatient setting, 59.9% and 83.8% of patients, respectively, had MDD as their primary diagnosis (p<0.001); 40.1% and 16.3% (p<0.001), respectively, had SI/SA as their primary diagnosis. The proportion of patients with a primary MDD diagnosis increased with LOS (short: 73.5%; medium: 89.6%; long: 92.0%; p<0.001). Increasing LOS was also associated with increasing utilization of the psychiatric unit (p<0.001). In the ED group, 54.2% were transferred to another facility and 43.9% were discharged home. A higher proportion (83.8%) of those treated in the inpatient setting were discharged home (p<0.001). Mean total hospital costs were $4,573 for all events, $753 for those in the ED group, $3,469 for short LOS admissions, $5,569 for medium LOS admissions, and $11,918 for long LOS admissions.
Conclusions: Characteristics of patients with MDD and SI or SA and hospital costs vary between those treated in the ED and inpatient setting, as well as across those with inpatient admissions stratified by LOS. Understanding patient characteristics by care setting and LOS may be informative for the development of more effective treatment strategies and the management of hospital resources.