Background: Patients hospitalized for major depressive disorder (MDD) with suicidal ideation (SI) or suicide attempt (SA) may have a high risk for hospital readmission. This study evaluated readmission/subsequent emergency department (ED) visit rates and the associated healthcare resource use and costs among patients who were hospitalized for MDD with SI or SA (SI/SA).
Methods: Patients ≥18 years of age diagnosed with MDD and SI/SA during an ED visit or inpatient admission were identified from the Premier Hospital database between 1/1/2014 and 6/30/2017. Patients were required to have either MDD as the primary and SI/SA as the secondary hospital discharge diagnosis, or SI/SA as the primary and MDD as the secondary hospital discharge diagnosis. The earliest admission or ED visit was defined as the index event. Patients were excluded if they had diagnoses of psychosis, schizophrenia, bipolar disorder, mania, or dementia. During a 6-month follow-up period after the index hospital discharge, all-cause as well as MDD-related and SI/SA-related readmissions/subsequent ED visits, were evaluated. Readmission and subsequent ED visit rates and associated hospital costs were evaluated for all patients and for those with ≥1 readmission/subsequent ED visit. Study outcome measures were stratified by inpatient LOS (categorized as short: 1-3 days; medium: 4-5 days; long: ≥6 days).
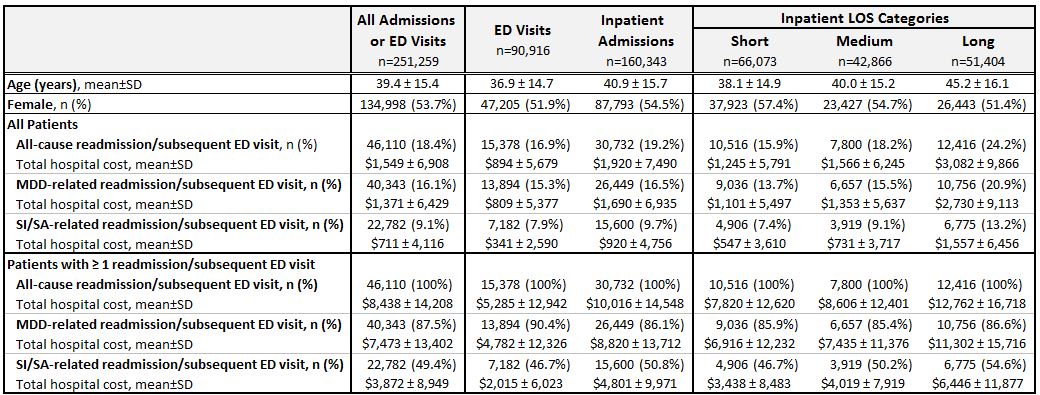
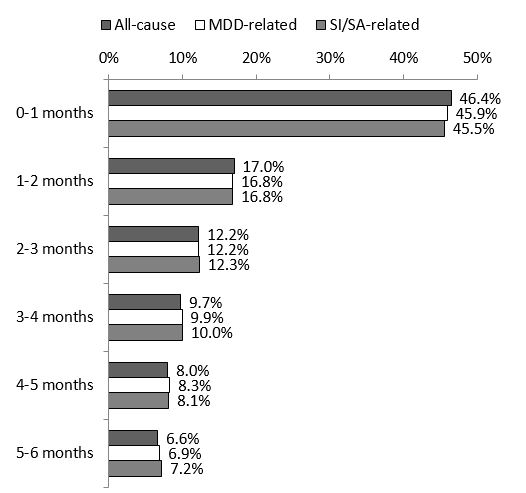
Results: Among the 251,259 patients (mean age: 39.4; female: 53.7%) with an index event, 46,110 (18.4%) had a readmission/subsequent ED visit for any cause during the 6-month follow-up period; 16.1% were MDD-related and 9.1% were SI/SA-related (Table). Among patients with readmissions/subsequent ED visits, 46.4% of all-cause, 45.9% of MDD-related, and 45.5% of SI/SA-related readmissions/subsequent ED visits occurred within 1 month of the index event (Figure). Rates of readmissions/subsequent ED visits and the associated hospital costs increased with longer index hospital LOS (Table). Among those with ≥1 readmission/subsequent ED visit, the mean all-cause total hospital costs per person associated with these events ranged from $7,820 to $12,762, for those with initial short and long stays, respectively.
Conclusions: These data document that readmissions/subsequent ED visits are not uncommon among patients previously hospitalized for MDD with SA or SI. In addition, a large proportion of readmissions/subsequent ED visits occurred in the first month after initial hospital discharge, which suggests an opportunity to improve patient outcomes and reduce costs.