Background: Concerningly, COPD exacerbations are the 3rd leading cause of readmissions nationwide, accounting for 60,000 readmissions annually. Patients hospitalized with COPD exacerbations have a 22.6% likelihood of readmission within 30 days, partially contributed to by their suboptimal disease awareness. However, there are educational tools that can be leveraged to improve treatment adherence, patient outcomes, and readmission rate.Through partnership with the REVISITS team, the purpose of our project was to decrease COPD readmissions through implementation of educational bundles. Our institution was one of about 20 sites participating in the REVISITS study, a program sponsored by the COPD Foundation and the Society of Hospital Medicine to reduce COPD exacerbation readmissions through educational interventions. We received mentorship from the REVISITS team but designed and implemented the interventions ourselves.
Methods: Patients who were admitted with a COPD exacerbation were enrolled in the 3-year intervention period starting in January 2023. The baseline data consists of 15 months (Oct 2021-Dec 2022) prior to the intervention period. During the index hospitalization, patients received a multifaceted educational bundle. The hospitalist reviewed their COPD medications and made edits as needed to optimize management and then created a COPD Action Plan (Figure 1). The COPD Action Plan mirrored features similar to those of the American Lung Association and was reviewed by nursing with the patient. Occupational therapy provided training in energy conservation techniques. The patients received an educational folder which contained COPD disease specific information, tobacco cessation resources, education about inhaler techniques, and information about pulmonary rehab enrollment. Finally, the patients were evaluated by the Transitional Care team who performed an after-discharge follow up call to review medications, review the action plan, and ensure appropriate follow up.
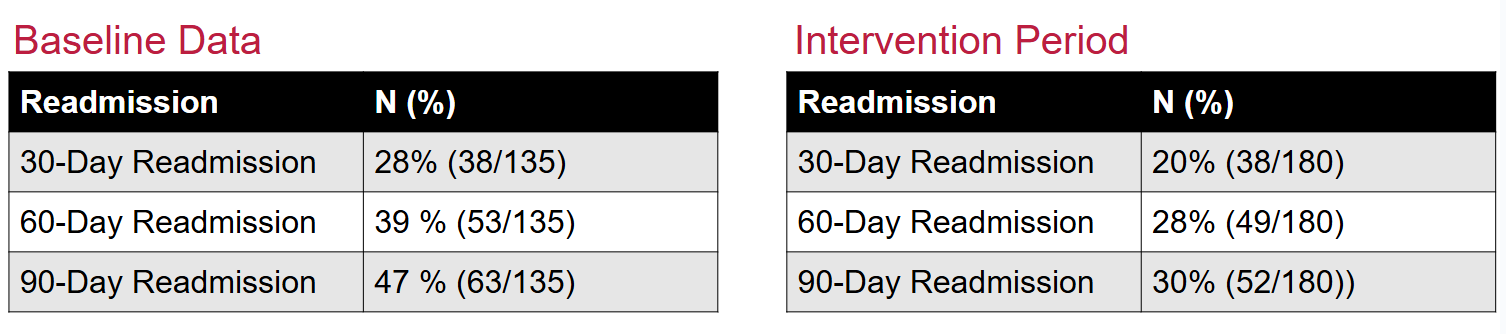
Results: After the index hospitalization, chart review was performed to determine the impact on readmission rates at 30, 60, and 90 days. When compared to the baseline period, the intervention period analyzed thus far from January 2023-May 2024 demonstrated a reduction in 30-day readmission rates from 28% to 20%, reduction in 60-day readmission rates from 39% to 28%, and 90-day readmissions from 47% to 30%.Through these interventions, errors in care have been identified and been corrected, including incorrect medication or inhaler choice, and lack of follow-up. Improved pulmonary rehab access could be of great value to patients as none of the patients who were seen by pulmonary rehab had readmissions within 90 days.
Conclusions: Our project demonstrates that with relatively simple educational interventions, patients with COPD exacerbations had fewer readmissions. With the focus on non-invasive educational opportunities, this can help augment patient understanding of disease and treatment options. Program goals include expanding to a broader scope across our institution. Beyond our work locally, it would be vital for the healthcare system nationally to recognize the impact that pulmonary rehab can have for these patients and work to expand access.