Background: A recent study showed over 80 percent of internal medicine residents reported being uncomfortable or very uncomfortable with dermatologic issues. Formalized teaching in dermatology in medicine residency may be prudent. This teaching could occur in both inpatient and outpatient settings. Our objective was to study the effect of a dermatology curriculum on knowledge and attitudes toward dermatology in an internal medicine residency program at an academic medical center.
Methods: The comprehensive dermatology curriculum was created using a curriculum map and aligning topics with appropriate venues. For example, Stevens-Johnson Syndrome was placed in the inpatient curriculum, whereas atopic dermatitis was included in the ambulatory curriculum. Medicine housestaff were invited to fill out a pre-intervention survey. Dermatology lectures were delivered by combined internal medicine and dermatology senior residents as well as dermatology faculty. Materials were also created to be posted on the housestaff website and distributed in lecture. Housestaff were then invited to fill out a voluntary post-intervention survey that was distributed via email 2 months after the last lecture in the curriculum. Surveys contained questions on self-reported attitudes and knowledge of dermatology and a 10-point objective knowledge assessment.
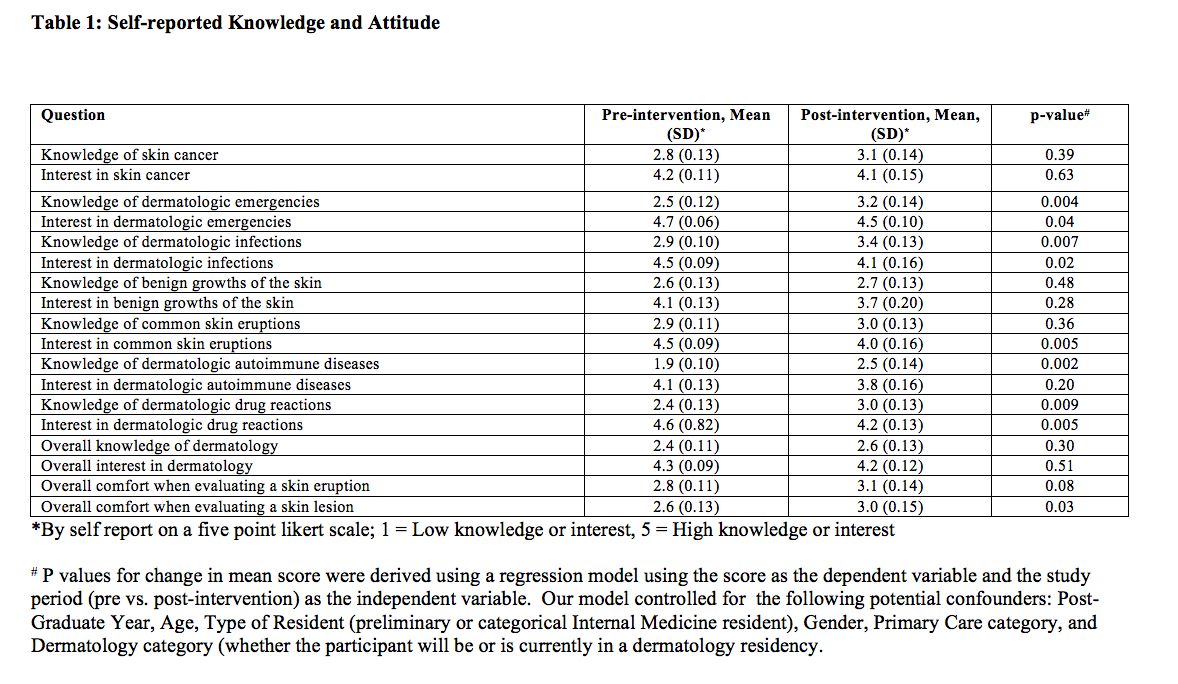
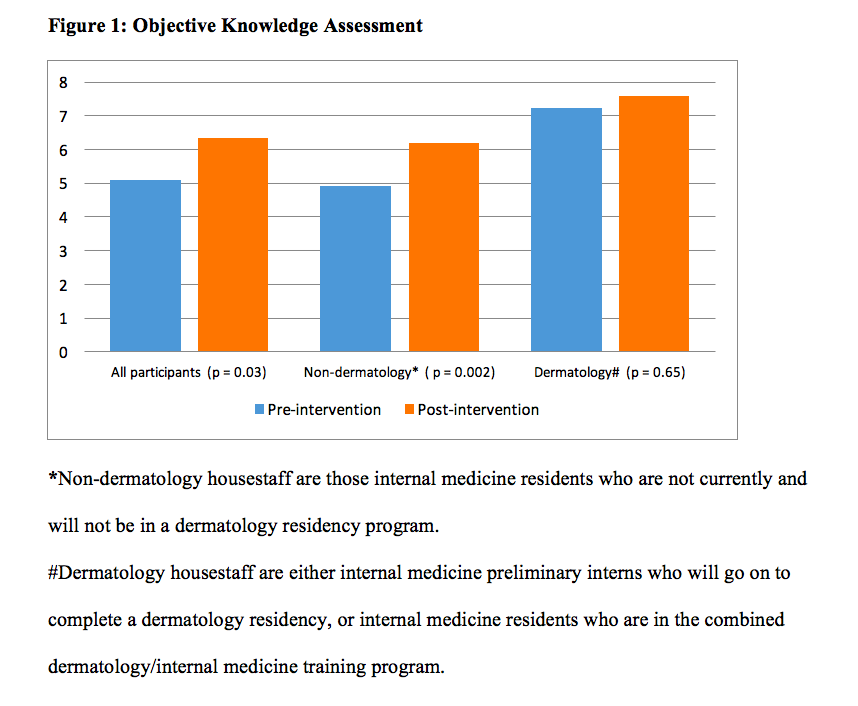
Results: 165 housestaff were invited to participate. 61 residents filled out the pre-intervention survey; 46 filled out the post-intervention survey. In multivariate analysis, the curriculum improved self-reported knowledge in dermatologic emergencies, skin infections, autoimmune diseases, and drug toxicities (p<0.05). The curriculum decreased self-reported interest in learning about dermatologic emergencies, skin infections, common rashes, and drug toxicities (p<0.05). There was increased comfort toward evaluating a skin lesion (p<0.05), but not a rash (Table 1). The curriculum improved scores on a 10-point examination from 4.88 to 6.33 (p<0.05). In subgroup analysis, this improvement in score was not demonstrated in housestaff who were either current or future dermatology residents, demonstrating specificity of this curriculum for non-dermatology housestaff (Figure 1).
Conclusions: The curriculum variably improved self-reported knowledge and decreased self-reported interest in a variety of topics. The curriculum improved scores on an objective knowledge assessment. This study suggests that internal medicine residency may be a potential venue for improving dermatologic knowledge for internists.