Background: The Improving Pediatric Patient-Centered Care Transitions (IMPACT) multi-site quality improvement collaborative aims to improve discharge transitions by use of a transition bundle, including use of a discharge checklist (DCL) to ensure completion of important transition tasks. These tasks included identification of a primary care provider, establishing follow up appointments, and ensuring access to medications, transportation, needed equipment and home nursing. Incorporating the checklist into the electronic health record delayed introduction at most IMPACT sites, but the aim of completion of checklist tasks was still pursued. Limited evidence exists about the effect of using a DCL or completing key tasks prior to discharge on hospital readmission in the pediatric setting. This study was undertaken to determine the effect of a completion of a DCL or its components on hospital reutilization in the pediatric setting.
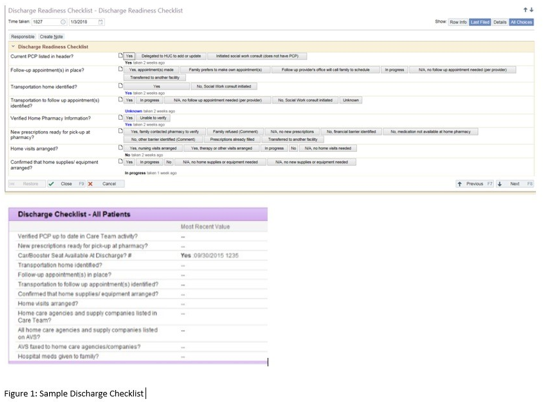
Methods: A DCL was developed based on expert consensus and literature review, with content including tasks identified as essential for safe transition to home (Figure 1). The DCL was introduced at IMPACT’s four pilot sites between 1/2014 through 8/2017. Charts were reviewed to determine demographic information, clinical risk group (CRG), checklist use and checklist component (DCL-C) completion. CRG was assigned using a previously published pediatric medical complexity algorithm into 3 categories; no chronic disease (CRG1), single chronic condition (CRG2) and complex/compound chronic condition (CRG3). Readmissions within 30 days were noted and readmission rates (RR) calculated. General effect and effect by site and CRG were analyzed using univariate (Chi Square) and multivariate analysis.
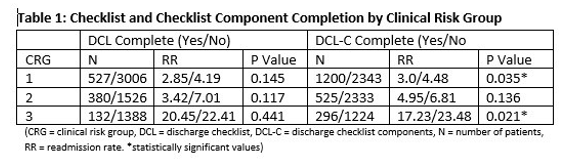
Results: Charts reviewed totaled 6963. Of those, DCL was completed in 1088; not completed in 5875. DCL-C was completed in 2030; not in 4933. Subgroup analysis by CRG revealed RR was decreased in each CRG for those with DCL completed, however the difference was not statistically significant. For those with DCL-C completed, RR was also decreased in each CRG, reaching significance for CRG 3. (p<0.017; see Table 1).Analysis of readmission by site and CRG independently showed a significant difference in RR for each (p<0.0001 for both).
Multivariate analysis of RR for CRG3 by site and DCL-C, confirmed the significance of checklist component completion for this population (p<0.017) indicating completion as a predictor of readmission.
Conclusions: Checklist use for pediatric patient discharge is associated with a decreased RR for all patients. The completion of key discharge tasks led to a significant decrease in RR for the most complex patients; this was confirmed by multivariate analysis. These results reinforce the importance of careful planning prior to discharge to ensure adequate patient and caregiver preparation, follow up, and access to needed supplies, equipment, and medications.