Background: Overuse of non-ICU continuous adult cardiac (telemetry) monitoring is a well-documented problem that can lead to increase hospital cost, alarm desensitization, nursing time loss, and patient discomfort 1,2. Previous studies assessing reduction of inappropriate telemetry use have employed a combination of electronic health record (EHR) order, nursing protocol changes, intensive educational, and/or feedback initiatives with varying degrees of success 2-4. Yet reproducibility and sustainability remains elusive given the resource intensive nature of many of these interventions and the lack of alternative monitoring for high acuity patients.
Methods: In this quasi-experimental, pre/post study, we sought out to determine if an EHR order with fixed time options and decisional support can reduce telemetry monitoring duration hospital wide and among hospitalist patients at a large academic hospital. We introduced a new telemetry order that incorporated the American Heart Association (AHA) and institutional expert opinion based indications, time recommendations, fixed time options, and a targeted alert for expired or expiring orders. The alert notifies ordering providers of expired or expiring orders during primary service hours (8am to 5pm) and prompts users to discontinue, renew, let expire, or modify the order. Primary outcomes were 1) proportion of prolonged telemetry orders (orders with durations >72 hours as a proportion of total telemetry orders, 2) total duration of telemetry orders before and after intervention. Secondary safety outcome was the proportion of rapid response and code events to total discharges (as a surrogate for hospital census), before and after intervention. Additionally, we looked at orders placed by hospitalist providers only. The new order with fixed time options and decisional support was implemented on June 6th 2019 and data were assessed for 7-months pre-intervention and 5-months post intervention.
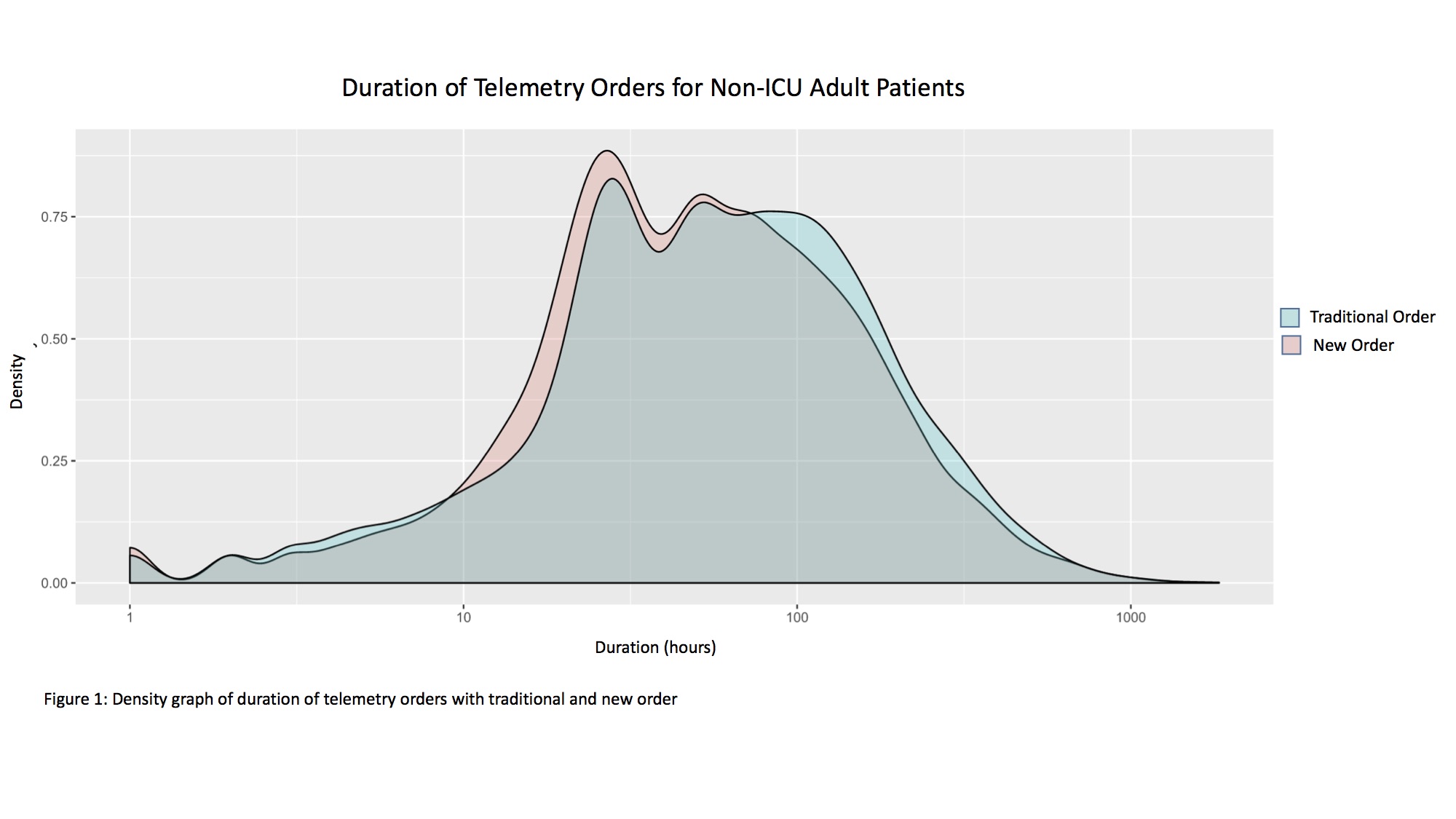
Results: Our dataset comprised 15616 telemetry orders under the traditional system and 12816 orders with decisional support (n = 28432). After the introduction of the new order, there was a significant decrease in the proportion of prolonged telemetry cases from 41% to 37% (Z = 7.5305, p = 0.00001 two tailed) for all non-ICU adult orders and a significant decrease of 50% to 42% (Z = 3.7902, p = 0.00016 two tailed) for hospitalist orders. Duration of telemetry for adult non-ICU patient was significantly shorter after the introduction of new order (Mann-Whitney U=124,347,965, p=2.2×10^-16 two-tailed) (fig. 1). We estimate that there was an average reduction of 5.6 hours per telemetry order (Hodges-Lehmann 95% CI: [4.6-6.7]). This was similarly seen in orders placed by hospitalist providers (average reduction 7.3, CI 2.2 to 12.6, W= 501313, p= 0.004566). There was a slight but significant decrease in proportions of rapid response and codes to total hospital discharges from 13.0% to 11.3% (Z = 4.3326, p = 0.00001). This suggest there may be unaccounted for differences in pre and post populations, but overall there was no increase in rapid response or code events after introduction of the new order with fixed time options and decisional support.
Conclusions: An EHR telemetry order with fixed time options and decisional support may be a safe and implementable option to decrease telemetry utilization and duration of telemetry monitoring in non-ICU adult patients hospital wide and among hospitalist providers.