Background: Regionalization of a provider team’s patients within dedicated nursing units has been shown to allow for improved efficiency and interdisciplinary collaboration. However, the creation of full regionalization is not feasible or appropriate for many medical centers given resource limitations. We hypothesized that we could achieve a significant increase in patient regionalization by modifying admitting and transfer protocols.
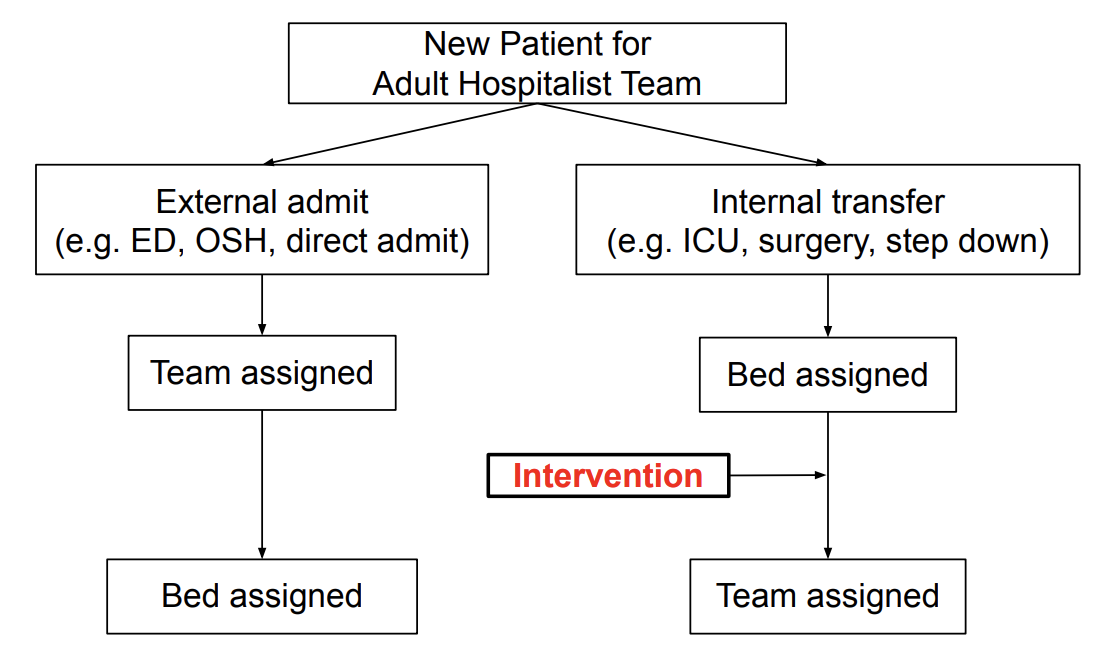
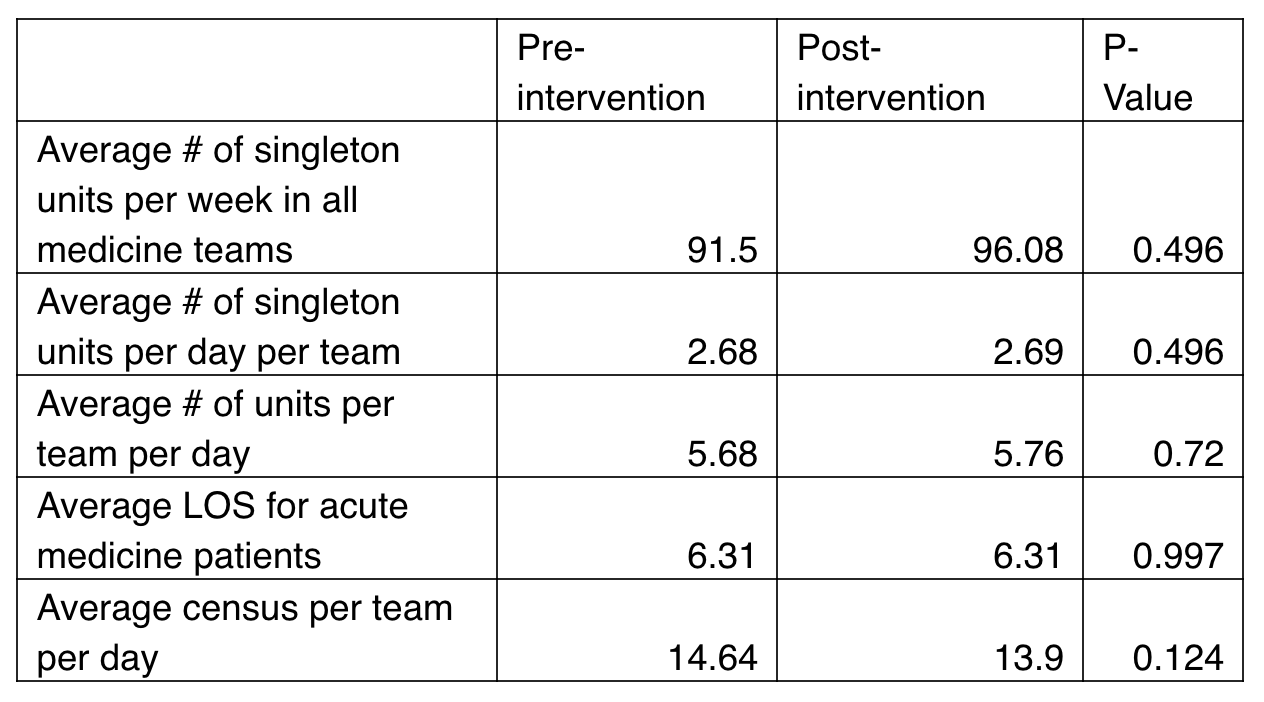
Methods: This study was conducted at a large Midwestern academic medical center involving 5 adult inpatient medicine teams, 3 teaching and 2 non-teaching. Specifically targeting inpatient transfers, we instructed the physician triage officers to use a modified protocol prioritizing patient regionalization when determining team assignment with the assistance of the bed-control personnel. Data was collected as automated reports from the electronic medical record for the 12 weeks before and 12 weeks after the intervention. The primary process metric was the number of “singleton” units, defined as units where a provider team had a single assigned patient at a given time- per week. Secondary measures included total number of units per provider team, and average length of stay for all patients in medicine services. We also measured patient census as a control. An unpaired, two-tailed t-test was used to compare endpoints.
Results: The average number of singleton units per day per team was 2.67 at baseline, while post intervention was 2.69 (p = 0.5). Implementation of our protocol did not result in a significant change in the number of singleton units or LOS for each team. During the study period there was no significant change in the patient census. Informal feedback received from the staff indicated poor compliance with the new protocol.
Conclusions: This study highlights the difficulties in implementing a protocol change that can impact key patient outcomes. Lack of buy in from frontline staff and poor compliance due to competing priorities was the biggest limitation of this intervention. We found that many structural processes including rigid call schedules for resident teams, need to keep a fair workload balance, bed availability among others created competing priorities in team and bed assignments. These competing priorities make regionalization on a large academic medical center very challenging. Moving forward we plan to create clear guidelines for when to prioritize team assignments over other competing interests, integrate the process of bed/ team matching into the workflow and shift responsibility from bed-control personnel to the physician triage officers.