Background: While the Coronavirus Disease 2019 (COVID-19) pandemic has substantially affected health outcomes globally, care strategies have varied in different regions. For example, while US hospitals primarily admitted patients with severe COVID-19, hospitals in Egypt admitted most symptomatic COVID-19-positive individuals per the May 2020 Ministry of Health and Population management protocol. Additionally, the use of therapeutics such as corticosteroids (CCS) and anticoagulant therapy (ACT) for COVID-19 treatment varied by geographic region. In this study, we aimed to compare how these variations in COVID-19 care strategies affected patient mortality between two US and Egyptian healthcare systems.
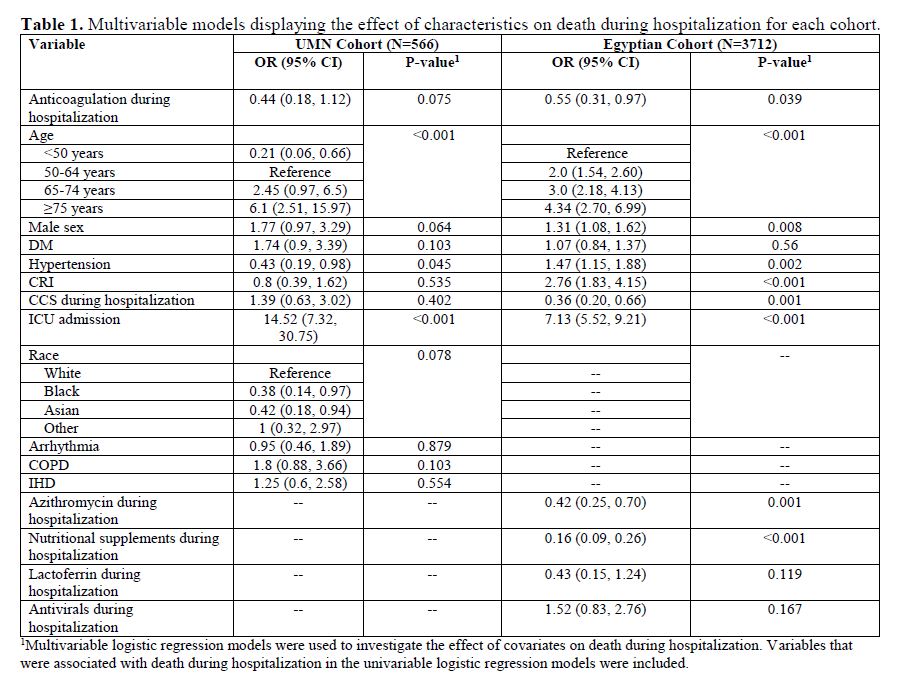
Methods: This analysis was performed as a multicenter, retrospective cohort study including patients from the University of Minnesota and multiple sites in Egypt. Patient demographics, comorbidities, mortality, thromboembolic events, and bleeding events were collected between March 1, 2020, and May 31, 2020, through electronic medical records (UMN Cohort) and patient files from four large volume centers in Cairo (Egypt Cohort). The primary outcome was mortality during hospitalization. The association between demographics, comorbidities, and ACT was investigated using Chi-square or Fisher’s exact tests. Multivariable regression models were used to investigate the effect of covariates on mortality.
Results: We included 4278 patients, 566 from the UMN cohort and 3712 from the Egyptian cohort. The percentage of males was similar in both cohorts, while more patients in the UMN cohort were ≥ 65 years old (45.6% vs.19.5%). Fewer in the UMN cohort received CCS (11.5% vs. 26.1%), and more of the UMN cohort received ACT than did the Egyptian cohort (83% vs. 39.6%). In-hospital mortality was 15.0% and 24.2% in the UMN and Egyptian cohorts, respectively. Our multivariate model exploring death during hospitalization demonstrated that ACT had a nonsignificant trend towards decreasing mortality for the UMN group and a significant reduction in mortality for the Egyptian group (UMN OR = 0.44, 95% CI: 0.18 to 1.12, P = 0.075; Egypt OR = 0.55, 95% CI: 0.31 to 0.97, P = 0.039). Similarly, CCS use had no significant effect on mortality for the UMN cohort and significantly reduced mortality for the Egyptian cohort (UMN OR = 1.39, 95% CI: 0.63 to 3.02, P = 0.402; Egypt OR = 0.36, 95% CI: 0.20 to 0.66, P = 0.001). Factors with a significant association with mortality for both groups included increasing age (UMN: ≥>= 75 years OR = 6.1, 95% CI: 2.51 to 15.97, P < 0.001; Egypt ≥>=75 years, OR = 4.34, 95% CI: 2.70 to 6.99, P < 0.001), hypertension (UMN: OR = 0.43, 95% CI: 0.19 to 0.98), P = 0.045; Egypt OR = 1.47, 95% CI: 1.47 to 1.88, P = 0.002), and intensive care unit admission (ICU) (UMN OR = 14.52, 95% CI: 7.32 to 30.75, P < 0.001; Egypt OR = 7.13, 95% CI: 5.52 to 9.21, P < 0.001). Additionally, the Egyptian cohort had increased mortality with the male sex (OR = 1.32, 95% CI: 1.08 to 1.62, P = 0.008), and chronic renal insufficiency (OR = 2.76, 95% CI: 1.83 to 4.15, P < 0.001).
Conclusions: Both cohorts demonstrated increased mortality with age and ICU admission. As expected based on clinical trials, the Egyptian cohort had reduced mortality with both CCS and ACT. The outcomes were different in the US cohort, perhaps owing to differences in patient population and medical practices.