Background:
The CURB‐65 score is widely used to risk‐stratify patients with community‐acquired pneumonia (CAP). When the score is less than 3, the patient is considered to have a low mortality risk, and current recommendations suggest that treatment may be provided in the outpatient setting. However, this tool only considers acute findings that reflect severity of illness; whether preexisting clinical conditions significantly alter the risk of adverse outcomes in pneumonia patients is unknown. Our objective was to evaluate the effect of comorbidities on clinical outcomes in patients admitted with low‐risk CURB‐65.
Methods:
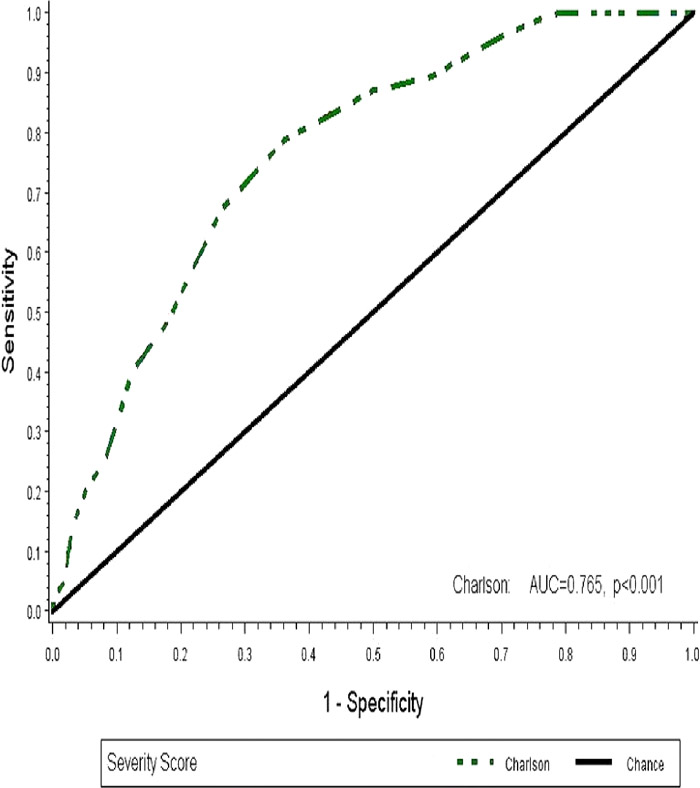
The medical records of consecutive patients admitted with CAP to a tertiary referral teaching hospital were reviewed to obtain the required clinical information to calculate the CURB‐65 score and the age‐adjusted Charlson Comorbidity Index (CCI). The performance of CCI in predicting 30‐day mortality was plotted on a receiver operator characteristic (ROC) curve, from which a cutoff value was derived to define low‐risk and high‐risk CCI. Patients with low‐risk CURB‐65 were stratified into low‐risk and high‐risk CCI. The rates of 30‐day mortality, 30‐day readmission, intensive care unit (ICU) transfer, and length of stay (LOS) > 7 days were compared between the 2 groups using chi‐square tests.
Results:
Five hundred and thirty‐eight patients were included in the analysis, of whom 399 (74.16%) had low‐risk CURB‐65. A CCI value of 7 was determined as the cutoff for the CCI risk groups based on the point of maximal sensitivity and specificity on the ROC curve for mortality. Of the patients with low‐risk CURB‐65, 269 (67.42%) had CCI scores less than 7 and were classified as low‐risk CCI, and 130 (32.58%) had CCI scores of at least 7 and were considered high‐risk CCI. The rates of 30‐day readmission and ICU transfer during the index admission were similar in both risk groups. The 30‐day mortality rate was 19.2% in high‐risk CCI and 4.5% in low‐risk CCI (RR, 4.31; 95% CI, 2.24–8.30; P < 0.001). Prolonged hospitalization (LOS > 7 days) was 35.4% in high‐risk CCI and 24.9% in low‐risk CCI (RR, 1.42; 95% CI, 1.04–1.94, P = 0.029).
Conclusions:
Among patients admitted with community‐acquired pneumonia with low‐risk acute clinical findings, the presence of preexisting comorbidities significantly increases the risks of mortality and of prolonged hospitalization. The age‐adjusted Charlson Comorbidity Index appears to be a useful tool in further risk‐stratifying patients who were identified to be low risk based on their CURB‐65 scores.
Rates of Clinical Outcomes in Patients with Low-Risk CURB-65 (Score < 3)
| Clinical Outcomes | Age-Adjusted Charlson Comorbidity Index | P Value | RR | 95% CI | < 7 (n = 269) | > 7 (n = 130) |
| 30-Day mortality | 4.5% (12) | 19.2% (25) | < 0.001 | 4.31 | 2.24–8.30 |
| 30-Day readmission | 14.9% (40) | 16.2% (21) | 0.738 | 1.08 | 0.67–1.76 |
| ICU transfer | 10.0% (27) | 14.6% (19) | 0.180 | 1.46 | 0.84–2.52 |
| LOS > 7 days | 24.9% (67) | 35.4% (46) | 0.029 | 1.42 | 1.04–1.94 |