Background: Guidelines by the Society of Critical Care Medicine and the Infectious Disease Society of America recommend empiric antibiotics active against Methicillin-resistant Staphylococcus aureus (MRSA) for certain patient groups but do not base their recommendations on systematic review or attempt to quantify the benefit on mortality.
Methods: A systematic literature search was conducted using Embase, Medline, PubMed, Web of Science, Cochrane, Scopus and Google Scholar from earliest entry through April 26, 2022. We included studies of patients hospitalized with culture-proven MRSA infections that compared mortality rates depending on whether patients received effective empiric antibiotics. The primary outcome was adjusted odds ratio for mortality.
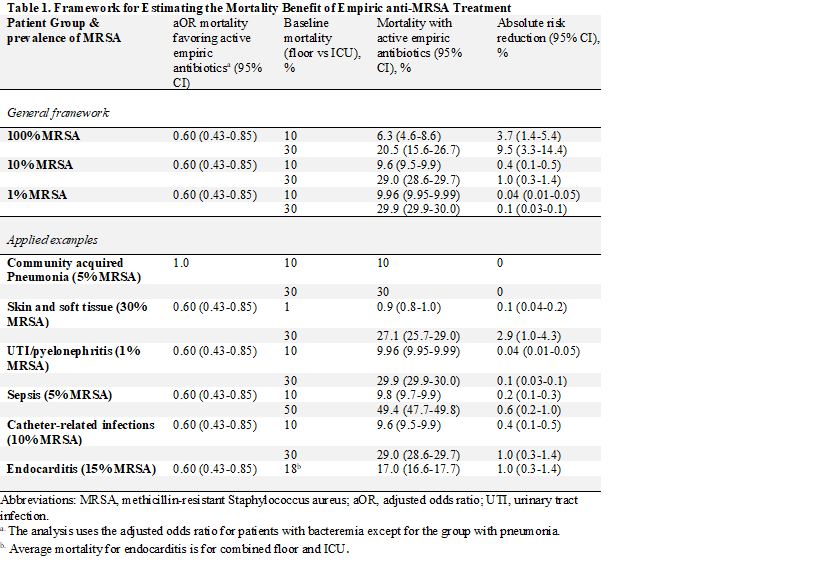
Results: We found 15 studies that reported adjusted odds ratios. The pooled mortality odds ratio was 0.64 (95% CI, 0.48-0.84), favoring active empiric antibiotics. Eleven of the 15 studies were of patients with bacteremia (aOR 0.60, 95% CI 0.43-0.85), two were of patients with pneumonia (aOR 1.56, 95% CI 0.74-3.27), and two were a mix of infection types (aOR 0.51, 95% CI 0.39-0.66). A framework was made to estimate the benefit for patients presenting with infection based on the probability of MRSA infection, the average mortality by infection type, and the benefit of active empiric antibiotics from the meta-analysis. The estimated absolute risk reduction was 0% for pneumonia, 0.1% (95% CI, 0.04-0.2) for soft tissue infections, 0.04% (95% CI, 0.01-0.05) for urinary tract infections, 0.6% (95% CI, 0.2-1.0) for septic shock, and 1.0% (95% CI, 0.3-1.4) for catheter-related infections.
Conclusions: For the three most common infections in the hospital the absolute benefit on mortality of empiric antibiotics against MRSA is 0.1% or less. Meaningful benefit of empiric antimicrobials against MRSA is likely to be limited to patients with approximately 30% mortality and 10% prevalence of MRSA, such as patients with septic shock or catheter-related bloodstream infections. Avoiding empiric antibiotics against MRSA for low-risk infections would substantially reduce the use of anti-MRSA therapy in the United States.