Background: In 2015, the United States had 25 million people with limited English proficiency (LEP). Most prior studies on disparities in outcomes in hospitalized patients with LEP compared to those with English proficiency were conducted outside the US and focused on outcomes such as hospital length of stay and mortality. There are also Emergency Department (ED) based studies that highlight increases in readmission rates and ED revisitation rates among patients with LEP who present to the ED. This study focuses on patients discharged from a hospital medicine service to examine the differences in rates of hospital readmission and ED revisitation, both of which are important measures impacting health care costs, health care quality, and patient satisfaction.
Methods: We conducted a retrospective case-control study using propensity matching at a quaternary care academic medical center. We included patients aged 18 years or older discharged alive from the Hospital Internal Medicine service from July 1, 2018 through July 30, 2021 in our initial sample. The population was then divided into two cohorts based on language status. Patients with LEP were defined as those who self-identified as needing an interpreter or where use of an interpreter was documented. The two cohorts were then propensity matched for age, sex, race, and Charlson Comorbidity Index (CCI). Our outcomes of interest were 30-day hospital readmission and 30-day ED revisitation rates between those with LEP and those who were English proficient. Comparisons between the groups were analyzed using conditional logistic regression.
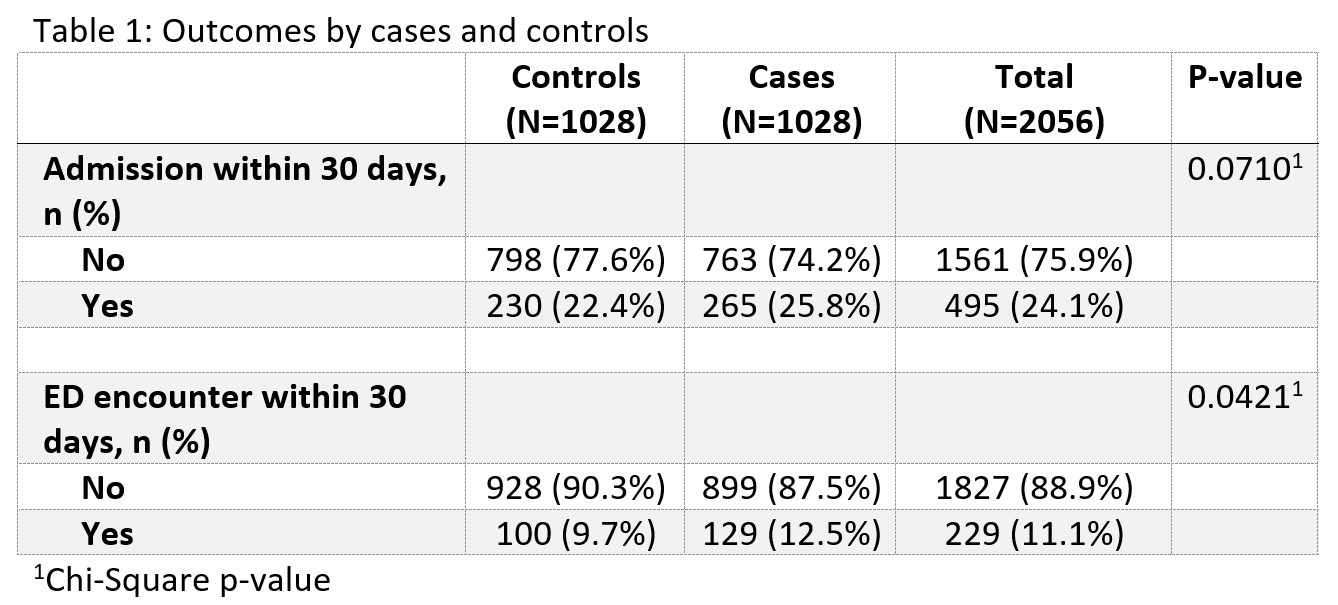
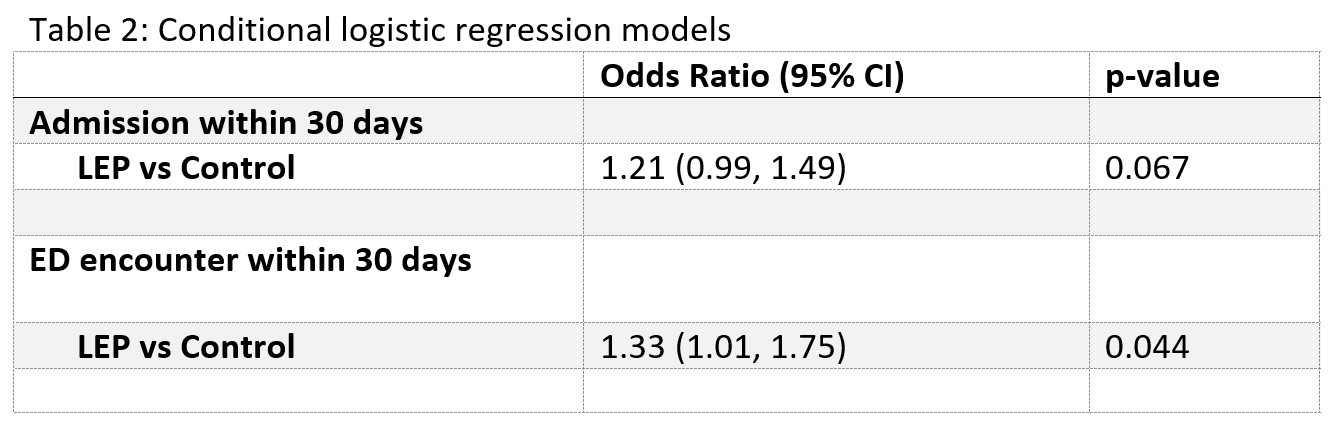
Results: A total of 158,265 patients met inclusion criteria during the study period. 2056 patients were propensity matched and included for analysis, 1028 patients with LEP (cases) and 1028 patients with English proficiency (controls). Tables 1 and 2 summarize the results and odds ratios of 30-day readmission and 30-day ED revisition between the groups. Overall 30-day readmission rates in these cohorts were 25.8% for patients with LEP and 22.4% for controls, however this difference was not significant (p-value 0. 0710). Patients with LEP had a significantly higher rate of an ED encounter within 30 days than the controls (12.5% vs. 9.7%, p-value 0.0421). In conditional logistic regression, patients with LEP had an odds ratio of 1.33 (95% CI 1.01-1.75, p-value 0.044) for 30-day ED revisitation compared to controls.
Conclusions: Patients with LEP were more likely to have an ED encounter within 30 days of discharge than controls. There was a trend toward increased rates of 30-day readmission for patients with LEP compared to controls, however this was not statistically significant. Our study was limited in power by small volumes of patients with LEP, which may have impacted our ability to detect differences. The small volumes and the inherent differences in the racial makeup between the two groups also resulted in incomplete matching by race. Given the diversity of the population of patients with LEP, more studies, especially multicenter studies, are needed to clarify health disparities that these patients experience to identify potential interventions to reduce these disparities.