Background:
In‐hospital adverse events such as unplanned intensive care unit transfers (UICUTs), cardiopulmonary arrests (CAs), and unanticipated mortality are frequently preceded by clinical instabilities. Rapid response systems (RRSs) have been advocated to detect and intervene on these instabilities with the goal of preventing serious adverse events. Although call criteria have been established based on retrospective analyses of patients’ clinical courses preceding in‐hospital adverse events, how well these criteria operate in practice is not known.
Methods:
We performed a search of major scientific databases and conference proceedings including Pubmed (MEDLINE), EMBASE, CINAHL, Cochrane Database, and Web of Knowledge through March 1, 2010, for studies using key words for RRSs. The quality of all studies was judged using prespecified criteria. Two independent reviewers using a standardized data extraction form extracted call criteria as well as event and call rates for each adverse outcome. In the initial stages of data analysis, we pooled the individual event and call rates from each study and used Bayesian statistics to determine the overall accuracy of call criteria by adverse outcome.
Results:
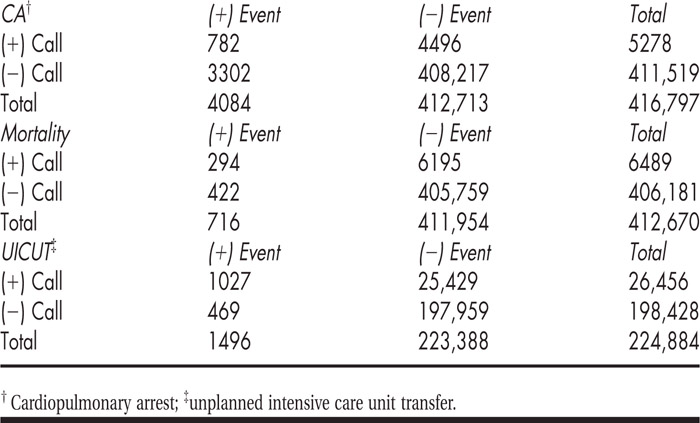
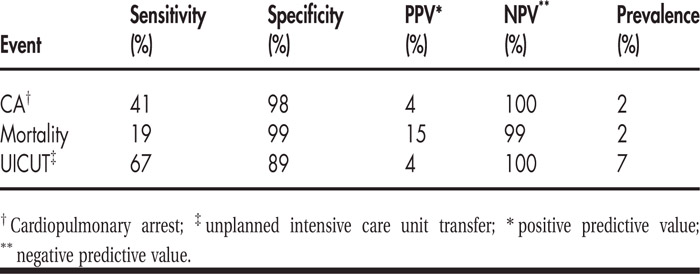
We retrieved 2197 citations based on a key word search. Of these, 13 studies representing 416,797 patients matched our screening criteria and were included. All 13 studies reported data for CA and unanticipated mortality. Only 7 of 13 studies reported data in UICUT. RRS calling criteria demonstrated significant heterogeneity. For example, respiratory rate criteria ranged from highs of 30–36/minute to lows of 5–8/minute. Preliminary results of pooled events and call rates are shown in Table 1. Operating characteristics of call criteria are shown in Table 2.
Conclusions:
Only 41% of CA and 19% of unexpected deaths are detected by rapid response screening criteria. Anywhere from 6.8 (mortality) to 25.6 (UICUT) calls are needed to prevent 1 adverse in‐hospital event because of a low positive predictive value (PPV). The low PPV of calling criteria may help explain why nurses often do not activate RRSs. Although attempts to improve the PPV by increasing the specificity of criteria would be limited by the concomitant decrease in sensitivity, screening a higher‐risk subset of inpatients would improve the overall performance of the call criteria. The poor real‐world operating characteristics of RRS calling criteria highlight the uncertain value of implementing RRSs to improve hospital outcomes.
Disclosures:
S. R. Bapoje ‐ none; P. S. Mehler ‐ none; R. K. Albert ‐ none; A. Sabel ‐ none; R. Bellomo ‐ none; S. Chandrasekaran ‐ none; E. S. Chu ‐ none