Background:
Limited access to interventional radiology (IR) services may delay placement of long‐term central venous catheters (LT‐CVCs). This can impair hospital throughput and escalate costs by increasing length of stay. We developed and implemented a hospital medicine procedure service to decrease delays in LT‐CVC placements.
Methods:
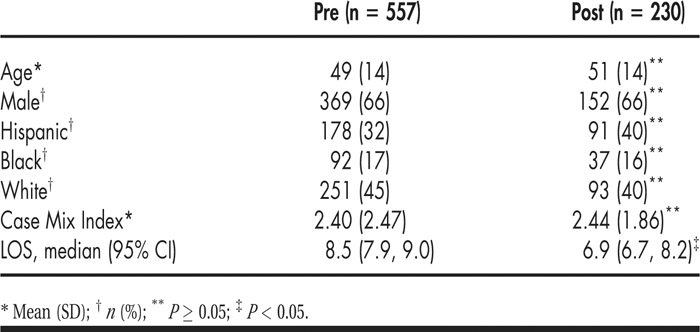
We performed a pre–post study at our university‐affiliated public safety net hospital. In spring 2009, a group of 6 hospital medicine proceduralists (HMPs) underwent a period of formal training by IR attendings in the insertion of LT‐CVCs (Hohn®) using the micropuncture technique and directed ultrasound guidance. HMPs started inserting LT‐CVCs in May 2009. We compared data from patients between 18 and 89 years of age who had single‐lumen LT‐CVCs placed by IR between May 2007 and April 2009, with those from patients in whom the LT‐CVCs were placed by HMPs between May 2009 and October 2010. Exclusion criteria included patients receiving triple‐lumen CVCs, CVCs placed while in the intensive care unit, and multiple placements of CVCs. We recorded demographics, the Diagnostic Related Group–based Case Mix Index, median length of stay (LOS) and complications, including central line–associated bloodstream infection, pneumothorax, and major bleeding (need for blood transfusion). Data from the 2 groups were compared using the Wilcoxon rank sum test. A P < 0.05 was considered significant. All analyses were performed using SAS Enterprise Guide 4.1.
Results:
Two hundred and thirty single‐lumen LT‐CVCs were placed by HMPs in the 18‐month intervention period (13/month) compared with 557 by IR over the 2 years prior (23/ month). Patients in the 2 groups were well matched (see Table 1). Median LOS was reduced by 1.6 days. In the 230 line placements, accounting for 1863 line‐days, no major complications (central line–associated bloodstream infection, pneumothorax, and major bleeding) were observed.
Conclusions:
Hospital medicine physicians can be trained to safely and efficiently place LT‐CVCs. When access to interventional radiology services is limited, LT‐CVC placement by hospital medicine proceduralists improves throughput.
Disclosures:
S. R. Bapoje ‐ none; R. Allyn ‐ none; M. Miller ‐ none; S. Stella ‐ none; D. Mancini ‐none; K. Angela ‐ none; R. Allen ‐ none; R. K. Albert ‐ none; E. S. Chu ‐ none