Background: Rapid response system (RRS) was developed in recent decades for the timely identification and treatment of clinically deteriorating patients. Appropriate use of RRS will decrease the incidence of cardiac arrest and mortality. Although efficacy of RRS was reported mostly in an inpatient setting, there were very limited data in an outpatient setting. The aim of this study is to investigate the effect of RRS in an outpatient setting.
Methods: This descriptive study was performed from April 1, 2014 to November 30, 2017 in a 350-bed referral hospital. We reviewed rapid response team (RRT) records, and cases from the outpatient setting were identified. Patients’ demographic data, activation trigger, intervention performed, time of arrival, disposition, and final diagnosis as well outcome were recorded.
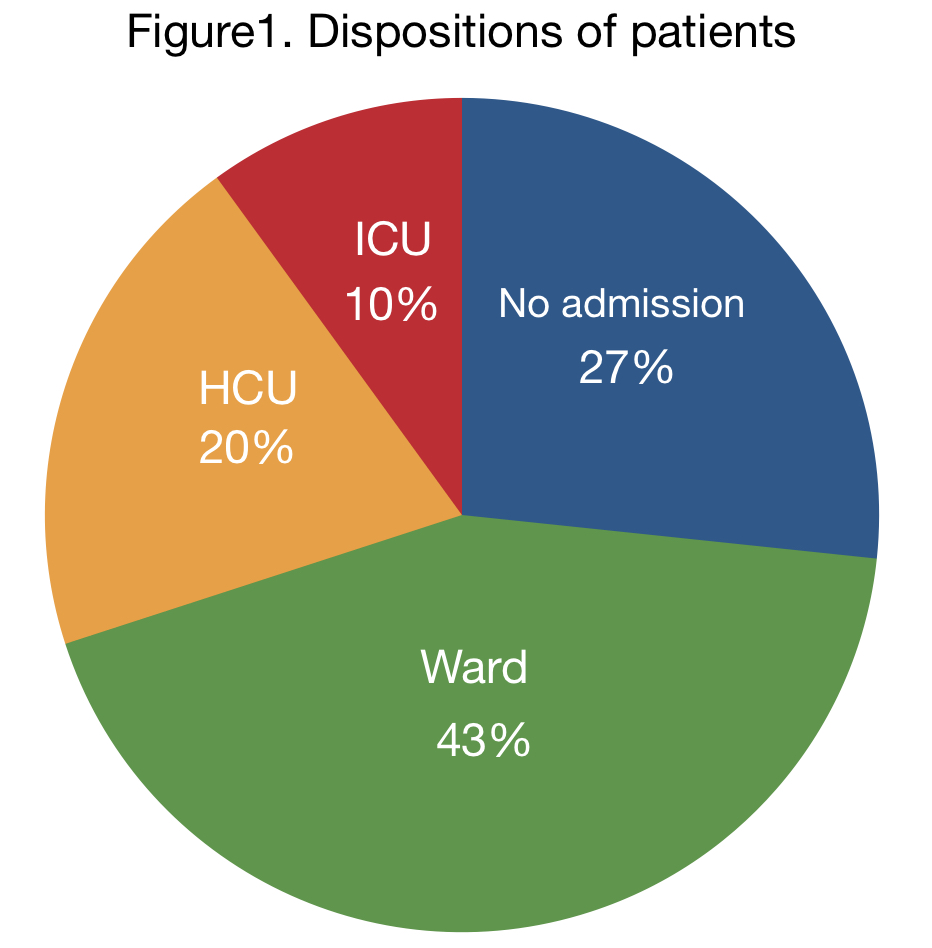
Results: There were 30 (male =22, female=8) outpatients for whom RRT was activated during the study period. The mean age (Standard deviation) was 62(19) years. All patients were transferred to emergency department, and evaluated by emergency physician-led RRT, according to our hospital RRT protocol. The median time interval from RRT activation to arrival of RRT was 5 minutes. The leading triggers for RRT activation were altered mental status (53%), tachypnea (40%), and hypoxemia (33%).The most common interventions performed included intravenous fluid (87%) and administration of oxygen (43%). One patient (3%) was intubated. Thirteen (43%), 6 (20%), and 3 (10%) patients were admitted to general wards, HCU, and ICU, respectively (Figure 1). Five (17%) patients received emergent endoscopy, and 2 (7%) patients (acute aortic dissection and ectopic pregnancy) underwent emergent operation.
Conclusions: Although lacking in control, RRS might possibly be effective even in an outpatient setting to identify outpatients who require prompt and timely evaluation and intervention.