Background: Traditionally, models of healthcare delivery to hospitalized patients have been indirect and inefficient. The typical hospital system has providers spread between multiple units and nurses interacting with multiple provider teams. Several studies focusing on interdisciplinary rounding (IDR) have shown a variety of positive impacts on hospital-associated metrics such as length of stay (LOS), hospital acquired infections (HAIs), and mortality. There are consistent reports of dramatically improved patient satisfaction, nursing staff satisfaction (with the benefit of reduced nursing turnover), and provider satisfaction.
Pioneered by Hospital Medicine providers at Emory, unit-based microsystems (Accountable Care Units – ACUs) are led by smaller teams of 2-3 semi-permanent physicians and dedicated unit nursing staff. The streamlining of responsibilities in this team-based model enables greater face-to-face communication between all members of the care team about the changing conditions and needs of their patients.
ACUs incorporate their team into daily structured interdisciplinary bedside rounds (SIBR) to keep rounds concise, transparent, up-to-date, and patient-centered. This model emphasizes real-time, meaningful, and compassionate interaction with the patient and their family at their bedside, while simultaneously promoting efficient teamwork and a culture of safety.This collaboration has been shown to improve patient outcomes at unit level, rather than hospital/health system level.
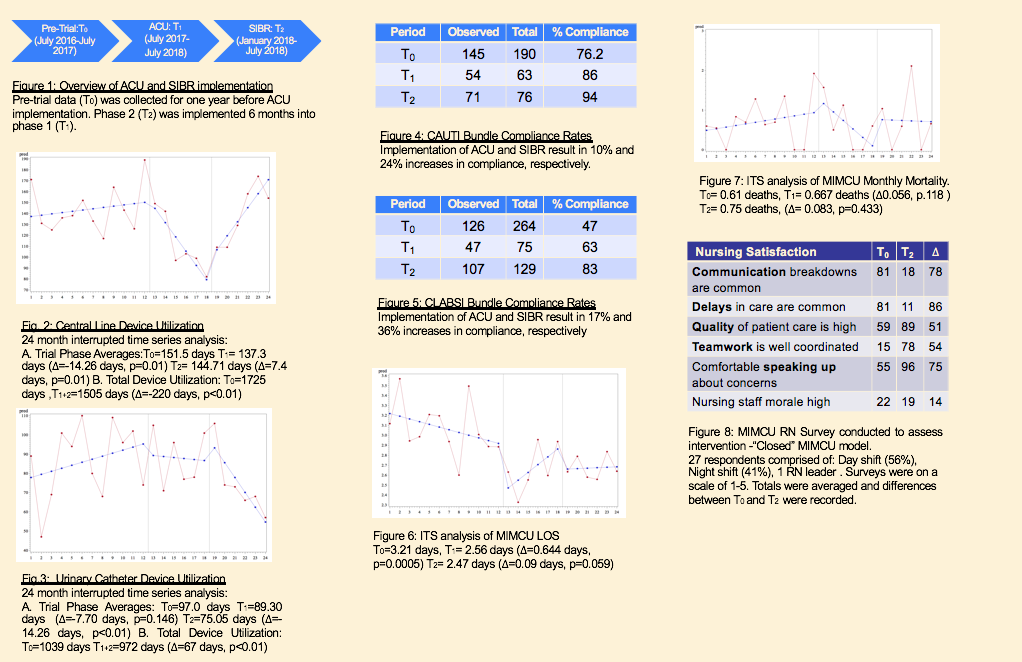
Purpose: A 20-bed Medical Intermediate Care Unit (MIMCU) was transformed into a geographic unit /ACU at our tertiary care academic medical center, effective 07/01/2017. The patients geographically assigned to the MIMCU were cared for by 2 general internal medicine teams. The teams were comprised of dedicated physician and nursing staff, consistent pharmacy presence, and unit specific therapy services (Speech Pathology, Physical Therapy, Occupational Therapy). SIBR was initiated 01/31/2018. Patient specific, deidentified reports were obtained for average length of stay and mortality, accounting for unit-specific and hospice-related mortality. Data was compiled to analyze Hospital-Acquired rates for Central-Line Associated Bloodstream Infection (CLABSI), central line device usage days, Catheter-Associated Urinary Tract Infection (CAUTI) rates, and urinary catheter device usage days. A retrospective survey was given to nursing staff to assess impact of the ACU framework on perceived culture of safety and working environment.
Description: Upon completion of the trial period, compared to baseline metrics, :
1. Central line/urinary catheter utilization significantly decreased (=-220 days, p<0.01/= -67 days, p<0.01).
2. CAUTI/CLABSI bundle compliance significantly increased (=+24%/=+36%).
3. LOS significantly decreased (=-0.65 days, p<0.001).
4. Nursing staff perception regarding work environment increased.
5. The MIMCU was recognized as having the highest patient satisfaction of any unit on the medical center’s campus for Q3 2018.
Conclusions: The data suggests that the ACU/SIBR framework provides a variety of positive benefits to patients and providers alike. While the data is promising, these findings represent a limited trial run at one medical center. Further investigation—including comparison to traditional models across multiple centers—is necessary to determine the feasibility of long term implementation and continued success regarding patient outcomes.