Background: eHealth interventions provide opportunities to enhance asthma or COPD self-management, though eHealth literacy (eHL) needs to be evaluated in this population. We evaluated the association between eHL and self-efficacy, as well as the willingness to use eHealth applications in patients hospitalized for chronic lung diseases (i.e., asthma and COPD).
Methods: This cross-sectional observational study surveyed adult inpatients from July 2018 to August 2023. Descriptive statistics, bivariate chi-squared analyses, and multivariate regression analyses (adjusted for age, gender, race, education, and technology access and use) were performed (STATA).
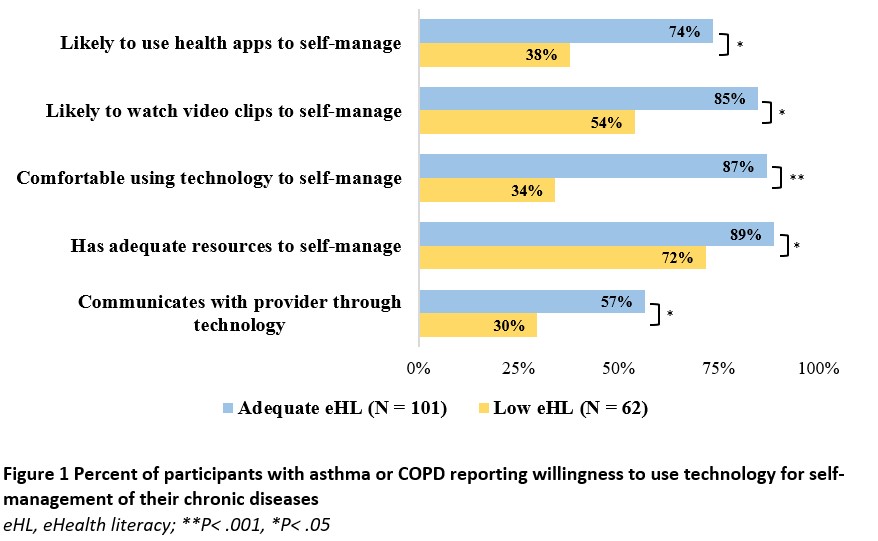
Results: Of 603 participants, the median age was 57 years; 68% identified as Black, 54% identified as female, and 28% were college graduates. Most (83%) had home internet access, while 34% had inadequate eHL. There was no significant difference in mean eHL scores between patients with (n=191) and without (n=412) chronic lung diseases (P=0.06). Most patients with chronic lung disease reported access to smartphones (n=131, 69%), while 42% owned a laptop or desktop computer (n=80). Half reported using the internet to access health information (n=96). The mean age was younger among users (51.2, SD=17.1) versus non-users (60.0, SD=15.5) of the internet for health information (P< 0.001). Among a sub-survey of patients living with asthma or COPD (n=93), most (82%; n=76) patients felt they had adequate resources to monitor their asthma or COPD and 65% (n=60) believed that their asthma/COPD was managed well at home. Reported asthma/COPD self-efficacy management was significantly associated with eHL (P=0.04). Specifically, self-efficacy was associated with knowledge of how to use resources on the Internet (P=0.02) and confidence in using Internet resources to make health decisions (P=0.03). Participants’ willingness to use health apps to manage their asthma or COPD was significantly associated with eHL (P=.001; Figure 1), ability to perform online tasks without assistance (P=0.04) and smartphone ownership (P=0.005). In simple regressions, all independent variables except for gender were significantly associated with eHL (P< 0.05). A multiple linear regression model explained approximately 53% of the variance in eHL scores (R2 adjusted = 0.527, P< 0.001). After adjusting for independent variables, the final model estimated that significant predictors of eHL included comfort with using technology for self-management (β=8.4, P< 0.001) and ability to use video without assistance (β=6.2, P=0.02).
Conclusions: Most hospitalized patients with asthma or COPD in our study access eHealth information and demonstrate willingness to use technology to manage their chronic diseases. Willingness to use health applications and reported self-efficacy in asthma or COPD management were significantly associated with higher eHL. Results of this study highlight the importance of evaluating eHL in considering equitable access to digital self-management resources and ensuring safe transitions of care.