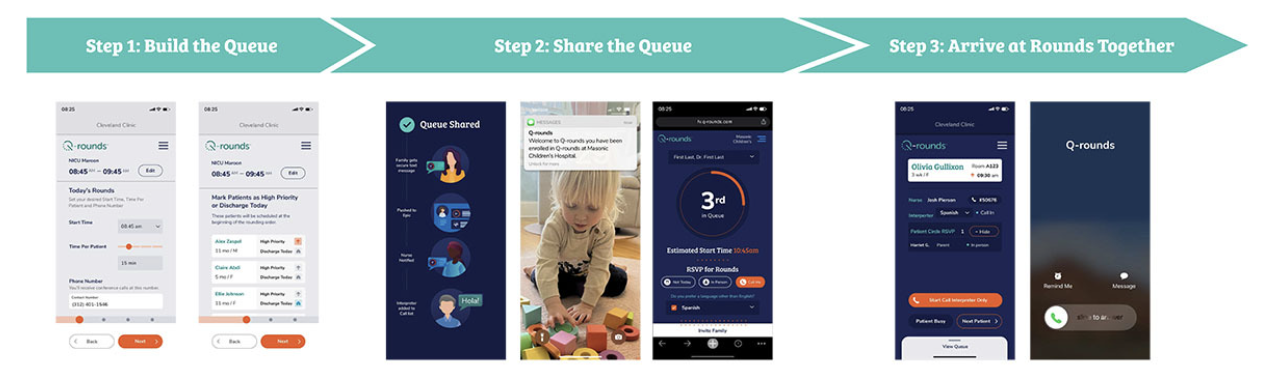
Background: In 2012, the American Academy of Pediatrics issued a statement recommending a standard practice for families and nurses to participate in rounds. Family-centered rounds (FCR) improves patient safety, patient and family satisfaction, provider satisfaction, interdisciplinary communication, and discharge planning. However, coordinating FCR in an easy and efficient manner to include all stakeholders remains a challenge. With the goal of increasing FCR, we developed a novel rounding software, Q-rounds, which provides text-based real-time updates to nurses and families of when to expect the rounding team. There is also an opportunity for families who cannot be there in person to RSVP to join rounds virtually (Figure 1).
Methods: We observed rounds in a 68-bed academic Level IV neonatal intensive care unit before and after implementation of Q-rounds on two rounding teams. The observations spanned twelve weeks (six weeks pre-implementation January-March 2023, a gap of 12 weeks, then six weeks post-implementation May-July 2023). Quantitative observational data was collected with a focus on relevant measures of interest regarding FCR: time spent per patient, nurse and family (in-person or by phone) presence and for what amount of time. The data was analyzed using a Chi-square test for categorical variables and two-group t-test for continuous variables.
Results: Rounds were observed for 165 patients (28.3 hours) in the pre-implementation period and 179 patients (31.0 hours) in the post-implementation period. Family presence for rounds increased from 20.0% to 43.0% (P<.0001) after implementing Q-rounds with 43 families choosing to join rounds virtually via Q-rounds during the 6 week post-implementation period. While the change in nurse presence for any part of rounds did not reach statistical significance (77.6% to 85.5%, P=.058), the proportion of nurses who were present for the entirety of the patients’ discussion increased from 18.8% to 58.2% (P=.0001). There was no change in the duration of rounds (10.3 minutes per patient before, and 10.4 minutes per patient after implementation; P=.91).
Conclusions: In the implementation of a novel rounding software, Q-rounds, we found improved rates of FCR with increased family involvement and time nurses are present for rounds without increasing rounding duration. The significant increase in family presence remotely when given the option suggests that families’ benefit from flexibility in the way they are involved in rounds.