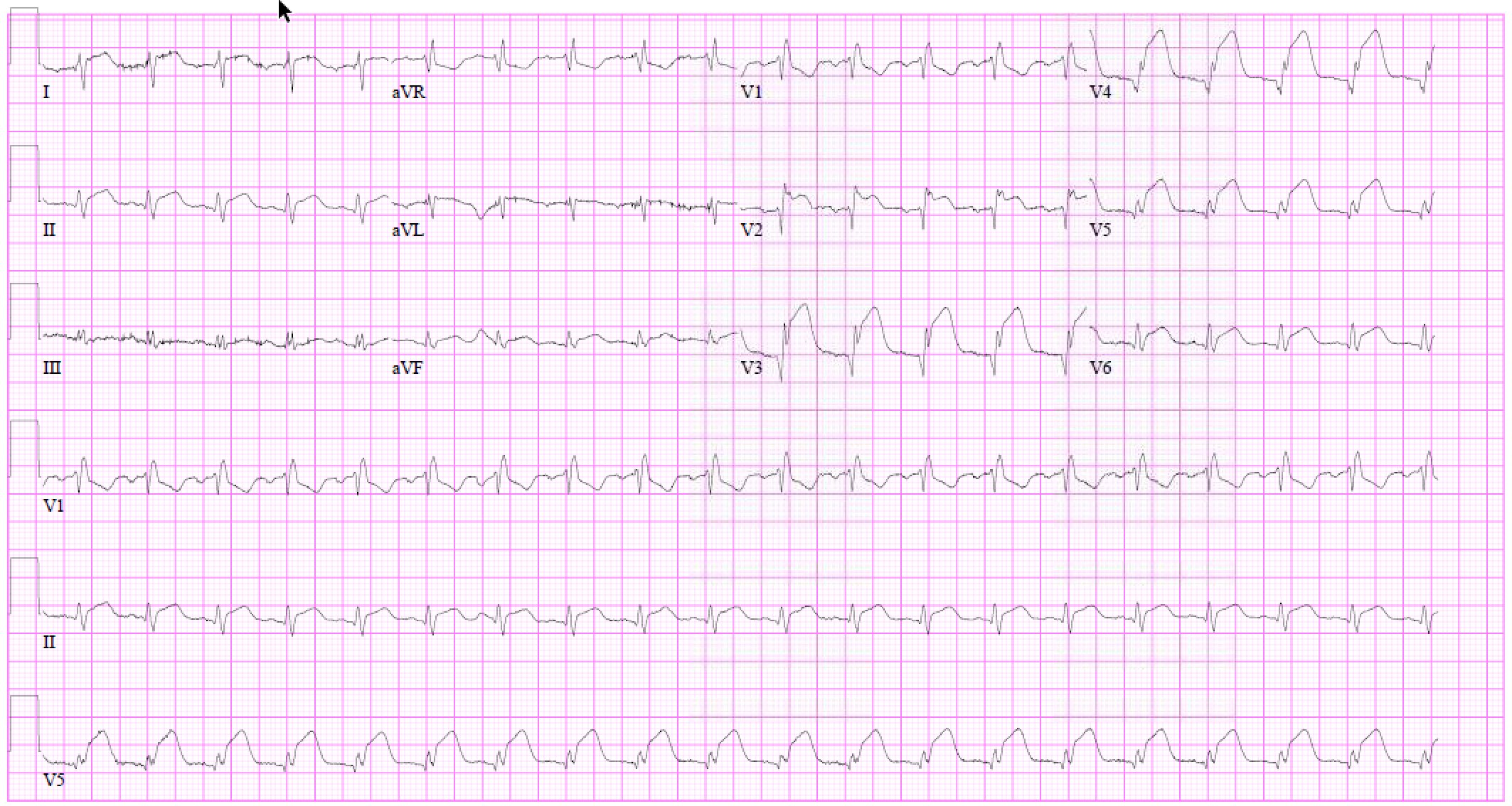
Case Presentation: A 38-year-old male patient with a history of intravenous drug use was transferred from an outside hospital after initial presentation with persistent fevers, episodic flushing and swelling in right hand and forearm. Workup at the other hospital included blood cultures positive for unspeciated yeast, and a transthoracic echocardiogram with normal ejection fraction (65%) and vegetations in right coronary cusp of the aortic valve with a diameter of 1.9cm. While awaiting surgery, patient developed acute chest pain with significant ST elevations in anterior and lateral leads, and troponin-I peak at 73.4ng/ml. A repeat echocardiogram was performed which reported severe reduction in ejection fraction to 25-30% and a vegetation attached to the aortic valve measuring 9mm x 9mm with size decreased compared to prior study. Apex, apical wall of the septum and the anterior wall were severely hypokinetic.Patient underwent debridement for abscess extending into interventricular septum with aortic valve replacement which was complicated by complete heart block leading to placement of permanent pacemaker. Due to patient’s history of intra venous drug use, he was discharged to a skilled nursing facility for the remainder of antibiotic duration.
Discussion: Acute coronary syndrome from Candida spp. is an extremely rare phenomenon. Myocardial ischemia is usually induced by coronary artery compression from peri-annular complications, and less frequently, an embolic infarct as in this case. Candida spp, namely albicans, account for the majority of these cases. Acute coronary syndrome in patients with infective endocarditis is associated with a higher incidence of heart failure, cardiogenic shock, complete atrioventricular block and mortality. Treatment involves intravenous anti-fungal agents followed by long-term suppressive anti-fungal therapy due to a high risk of recurrence. Thrombolytics, balloon angioplasty and stent placement have been attempted but aspiration thrombectomy appears to be a safer approach.
Our patient did not undergo left-heart catheterization and was medically managed for his myocardial infarction. Patient has since been following with cardiology and infectious disease outpatient clinics, and was re-admitted with fever and found to have multiple saccular aneurysms of hepatic, superior mesenteric and left femoral arteries, and a psoas abscess with failed attempt at drainage by interventional radiology. He is maintained on life-long fluconazole as he continued to have positive 1-3 ß-D-glucan levels without episodes of breakthrough candidemia.
A repeat trans-esophageal echocardiogram performed ten months after initial episode ruled out recurrent endocarditis. Patient has since developed ventricular desynchrony and was upgraded to biventricular implantable cardioverter defibrillator.
Conclusions: In summary, septic coronary embolization from candida endocarditis is an extremely rare phenomenon which is associated with poor clinical outcomes. Treatment involves intravenous followed by long-term suppressive oral anti-fungal therapy. Role of percutaneous interventions requires further investigation with prospective randomized control trials.