Background: Epipericardial fat necrosis (EFN) presents as acute chest pain with the potential to mimic life-threatening conditions. It is unclear whether this is truly a rare condition, or simply underdiagnosed by low threshold of suspicion. The literature suggests an estimated prevalence of 2% of EFN as the cause of chest pain in all patients presenting to the emergency department with such complaint.
Methods: We performed a systematic review of the literature of electronic databases (PubMed, Embase, LILACS, SciELO), resulting in 63 case reports of EFN from a total of 55 articles. We included the terms “epipericardial fat necrosis”, “pericardial fat necrosis”, “mediastinal fat necrosis”, and “epicardial fat necrosis”, as well as their corresponding translations in Portuguese and Spanish. We followed the PRISMA guidelines when conducting this systematic review.
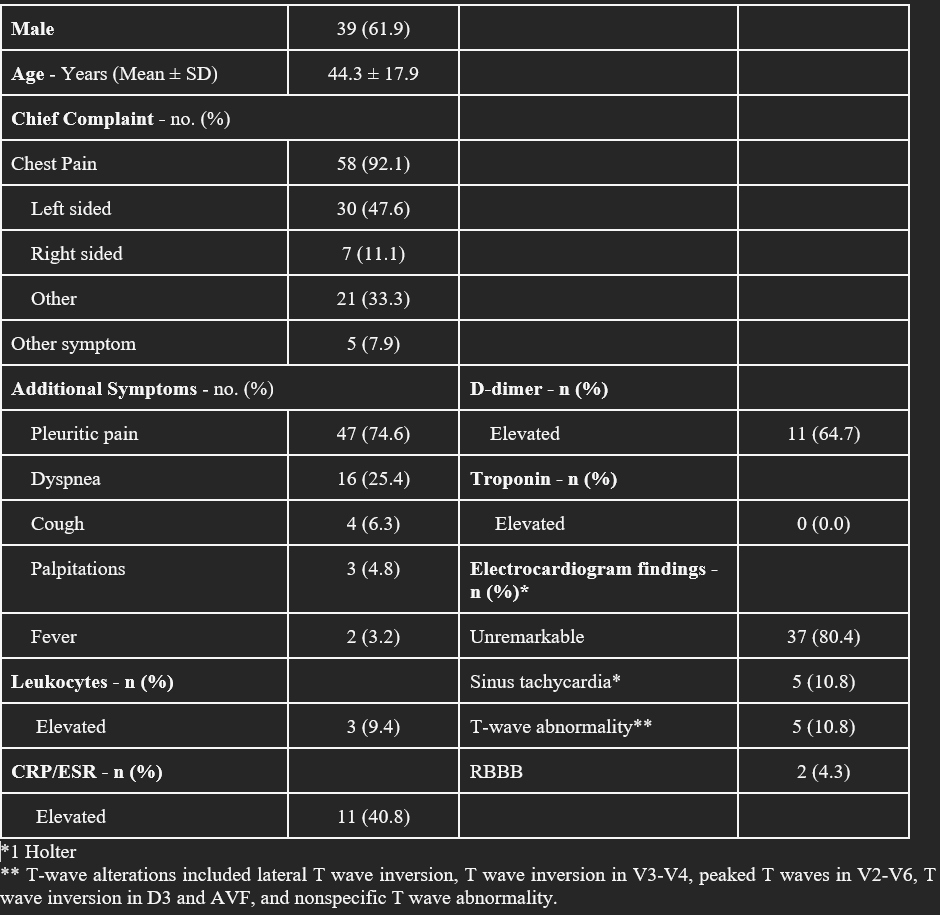
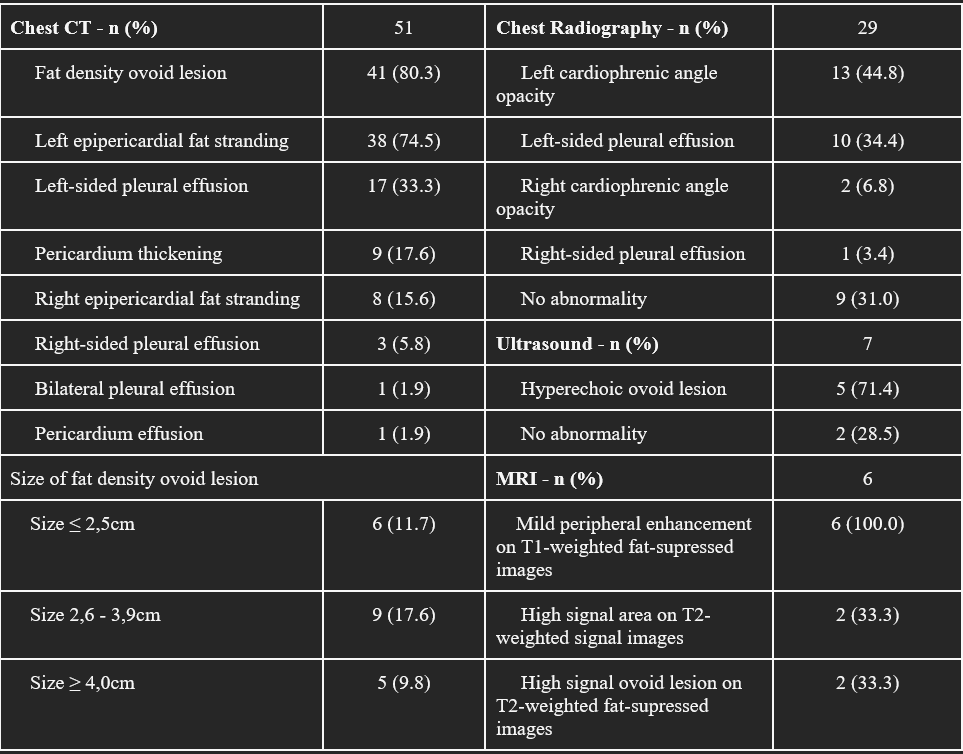
Results: 142 articles were found following an initial search. 87 articles were excluded based on inappropriate study design, duplicate reports, language other than the included in this review and incomplete data. We encountered that EFN usually presents in middle aged patients, with a chief complaint of chest pain in over 90% of the cases, most commonly left-sided. The pain is most often characterized as pleuritic, and the most common accompanying symptom is dyspnea, occurring in 25.4% of the cases. Notably, biochemical work-up and ECG are usually unremarkable and the diagnosis is confirmed via chest imaging. Although chest X-ray and echocardiogram may provide useful clues, chest computed tomography (CT) scan or magnetic resonance imaging are necessary to confirm the diagnosis. The assessment of patients with EFN starts with ruling out more serious and life-threatening conditions. In our review, we have found that all reports investigated acute coronary syndrome, and all patients presented with negative troponin results. As the epipericardial layer of fat tissue outside the visceral pericardium has blood supply from non-coronary sources and does not directly involve the myocardium, this was an expected and reassuring finding for this type of necrosis. Regarding the natural history of the disease, EFN appears to be a benign entity with low mortality and morbidity. Among the 52 patients with reported outcomes, we encountered 7 patients who underwent surgical treatment and 45 managed conservatively. All had resolution of symptoms and no reported sequelae. Indeed, we encountered only one report of a serious complication of pericardial tamponade following surgical treatment. In the 39 (84.7%) patients managed pharmacologically with analgesics and anti-inflammatory drugs, all experienced favorable outcomes. No patient died or had any sequelae from this condition in the short-term follow-up.
Conclusions: EFN is an underdiagnosed benign condition that presents with acute chest pain, rely on chest imaging for its identification, more specifically CT of the chest. Conservative treatment with NSAIDs or common analgesics is a reasonable and acceptable approach to manage patients, considering the benign course and prognosis of this entity. A high degree of suspicion is required in order to avoid further invasive work-up and management.