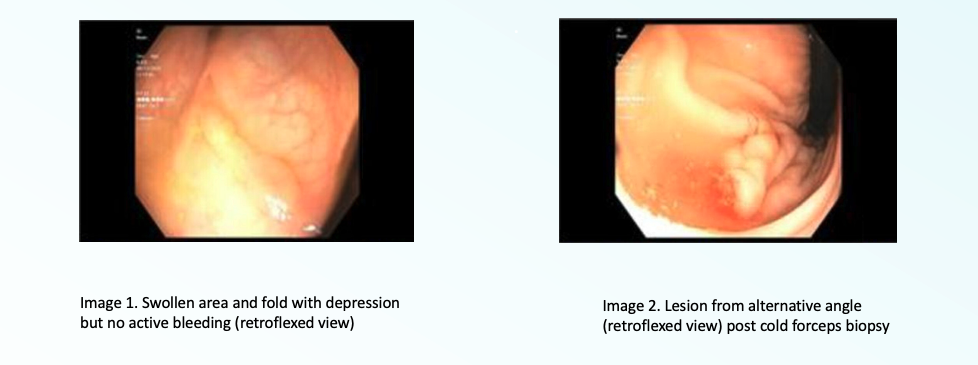
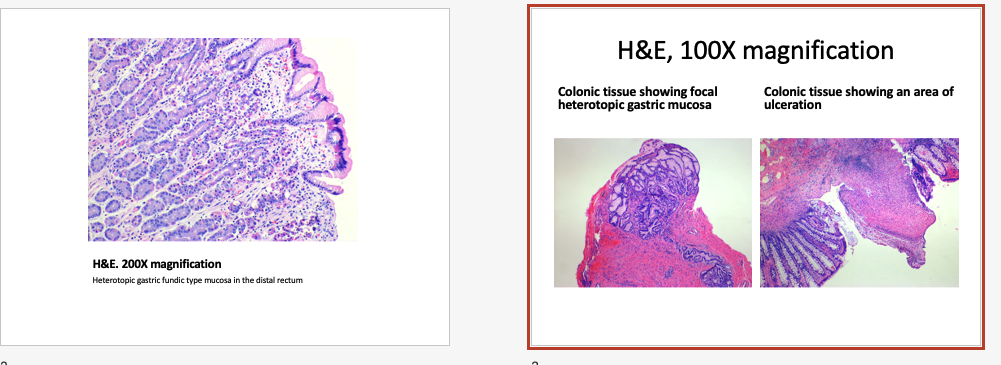
Case Presentation: A 10-year-old female presented with her third episode of painless hematochezia. Episodes were separated by months, each lasting 3 to 5 days with passage of multiple “fist-sized” bright red clots. There were no other associated symptoms and resolution of bleeding was spontaneous. Extensive prior workup included coagulation studies, upper and lower gastrointestinal (GI) endoscopy, capsule endoscopy, abdominal Computerized Tomography angiography, mesenteric three vessel angiography, tagged red blood cell scan, Meckel’s scan and exploratory diagnostic laparoscopy. The only abnormality detected was dysplasia of the descending colon arteries on angiogram, which was later determined to be incidental.The patient’s physical exam upon admission, including rectal exam, was normal, guaiac was negative, and no further bleeding occurred. Differential diagnoses included Meckel’s diverticulum, arteriovenous malformations, polyps, and diverticula. Due to prior history, work-up ensued.Blood counts and coagulation labs were normal. A tagged RBC scan was repeated and normal. Colonoscopy was undertaken. The study was unrevealing until the scope was retroflexed and an abnormal fold and depression near the rectum was visualized. A surgical biopsy of this tissue was obtained, and pathology revealed ulcerated gastric heterotopia. A pill capsule study was repeated and showed an additional bleeding in the jejunum. The patient was started on acid suppression for multifocal ulcerated gastric heterotopia. She underwent excision of the rectal lesion. At discharge, minor rectal bleeding persisted, as expected post-operatively. Following discharge, the patient was lost to follow-up.
Discussion: The term heterotopia refers to the presence of normal tissues at foreign sites. Gastric heterotopia has been reported throughout the GI tract with an endoscopic prevalence in the fore- and mid-gut ranging from 0.1% to 11%(1), however presence in the rectum is very rare(2). Gastric heterotopia commonly presents with painless lower GI bleeding and may be associated with polyps, diverticula, or ulcers. Definitive diagnosis may require repeat evaluation in the setting of acute bleeding to improve test sensitivity, particularly with visualization via endoscopy. Early identification of rectal lesions is crucial given their association with major GI bleeding, intussusception, and recto-vesicular fistula. Acid suppression therapy can significantly improve rectal bleeding, however mucosal abnormalities remain, and bleeding recurs if medications are stopped. Rare reports of esophageal heterotopic lesions resulting in adenocarcinoma suggest a concern for malignant transformation for all heterotopic lesions, underscoring the importance of surgical resection when lesions are accessible. Surgical resection is curative.
Conclusions: Rectal heterotopic gastric mucosa should be considered in the differential diagnosis of an obscure GI bleed. While rare, a high index of suspicion should be maintained to avoid complications including massive GI bleed, intussusception, and malignant transformation. Although acid suppression therapy improves symptoms, surgical resection is required to ensure a complete cure.