Background: Over 5 million hospital-to-skilled nursing facility (SNF) transitions occur annually. Of these patients, 20% are readmitted within 30 days, and 25% of those readmissions are deemed preventable. While effective communication between the inpatient clinician and the accepting SNF clinician has been shown to improve re-hospitalization rates, few studies have examined clinician confidence or competence with SNF handoffs. We aimed to measure resident discharge teams’ and accepting SNF clinicians’ knowledge, attitudes, and satisfaction with the SNF discharge process.
Methods: We surveyed medicine residents at an urban academic medical center and SNF providers at three urban SNFs. Resident surveys measured self-reported level of knowledge and confidence with SNF handoffs. SNF provider surveys gauged their ability to find needed information for a safe transition of care (e.g. hospital summary, medication reconciliation, wound recommendations) in the received verbal hand-offs and discharge summaries. Surveys were distributed via email and also available to residents via QR code displayed at conference multiple times per week.
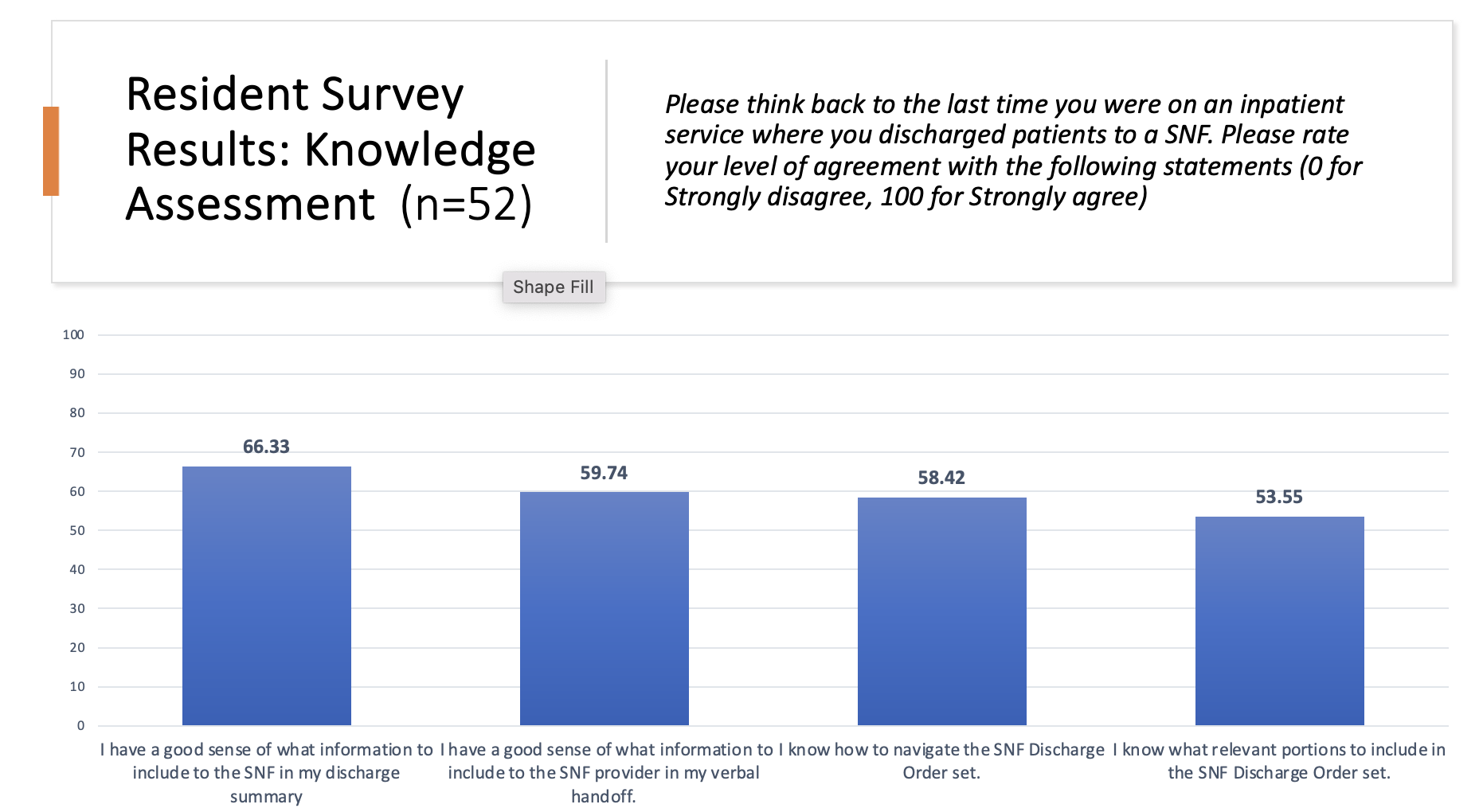
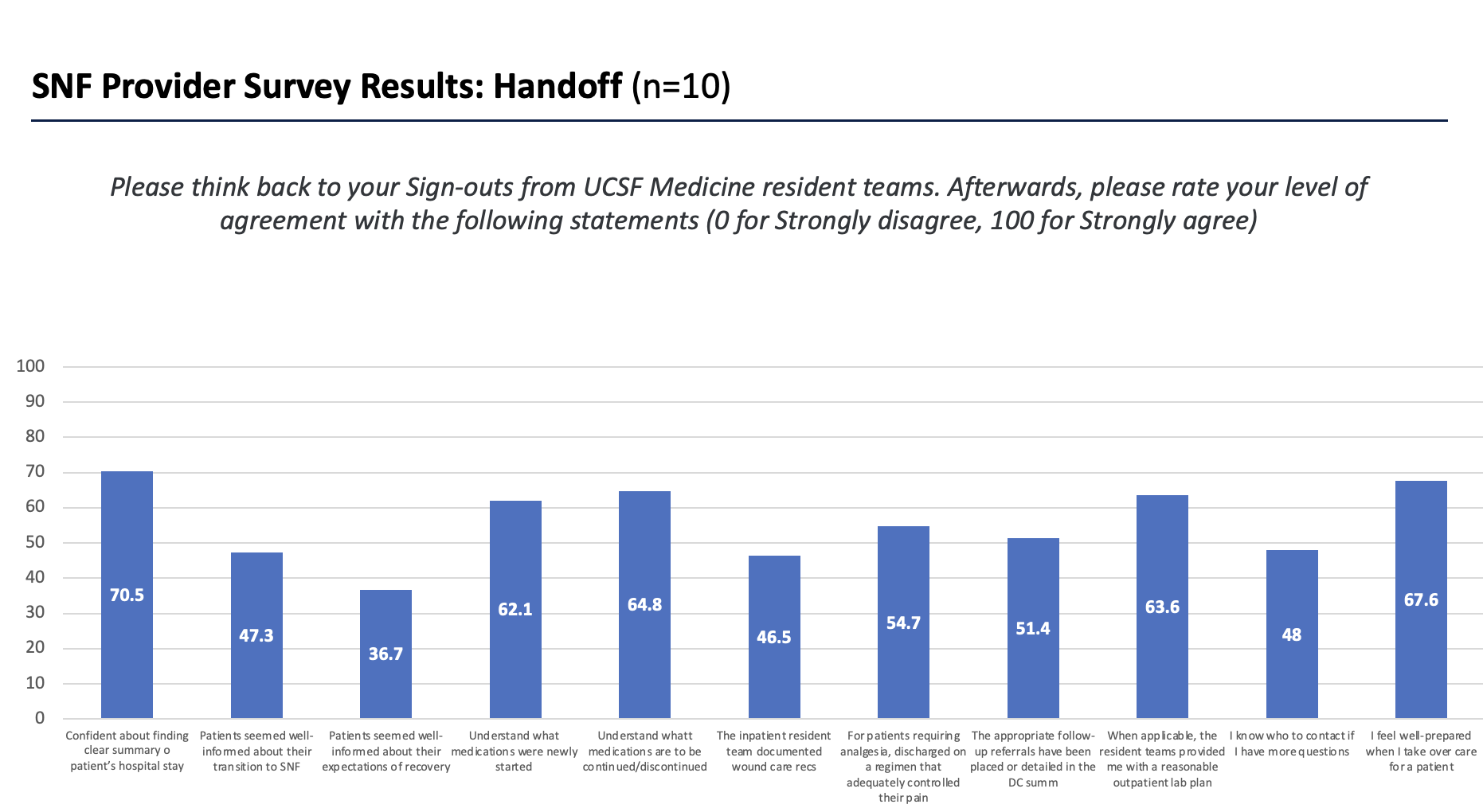
Results: Surveys were distributed to 184 residents and 10 SNF providers, with 28.3% (n= 52) and 100% (n= 10) response rates, respectively. Residents were only 59% confident in knowing what information to include in the SNF discharge handoff. Residents infrequently provided guidance on wound care recommendations (44%) or Foley catheter management (42%), and only listed a contact number (for SNFs to use if there were concerns) 51% of the time. Conversely, SNF clinicians were only 47% confident in being able to find wound care recommendations and 48% confident in knowing who to contact if they had questions post-discharge. Only 47% of SNF doctors thought patients had been well-informed by residents about their transition to SNF, and 37% of SNF providers thought patients had a good understanding of their overall recovery process. In the open responses, 40% of SNF clinicians mentioned medication reconciliation as an area of improvement.
Conclusions: We identified a current gap in knowledge and consistency in the communication and documentation of hospital-to-SNF transitions. Residents lack understanding about SNFs, which may contribute to uncertainty about what information to include in handoffs and low confidence in counseling patients on what to expect when discharging to a SNF. Meanwhile, SNF providers are currently only moderately confident in their ability to take over care after receiving a patient from the hospital because crucial information is not clearly communicated in the hand-off or discharge summary, particularly medication changes. Having SNF provider input on what is important to include and standardization of the SNF discharge process for residents might help make this complicated transition of care safer.