Background: In the hospital care setting, clinician groups employ a range of staffing models utilizing physicians as well as advanced practice providers (APPs), to meet patient care needs. Models have evolved in recent years in part due to pandemic related staffing constraints; proposed policy changes to billing practices may also be contributing. The Centers for Medicare and Medicaid Services (CMS) previously announced plans to change billing rules for inpatient visits that are shared by physicians and APPs whereby the clinician spending the most time (greater than 50%) on the patient visit would bill services for the visit.
Methods: To understand how inpatient hospital medicine teams utilize APPs in patient care and how billing policies might impact future APP utilization, we conducted focus groups with hospitalist physicians, APPs, and other leaders across 21 academic institutions through the Hospital Medicine ReEngineering Network (HOMERuN) collaborative. Using rapid qualitative methods, six semi-structured focus groups were held virtually, and audio files were analyzed using a mixed inductive and deductive method at the semantic level with templated summaries and matrix analysis. A brief REDCap survey was also included at the beginning of the focus group.
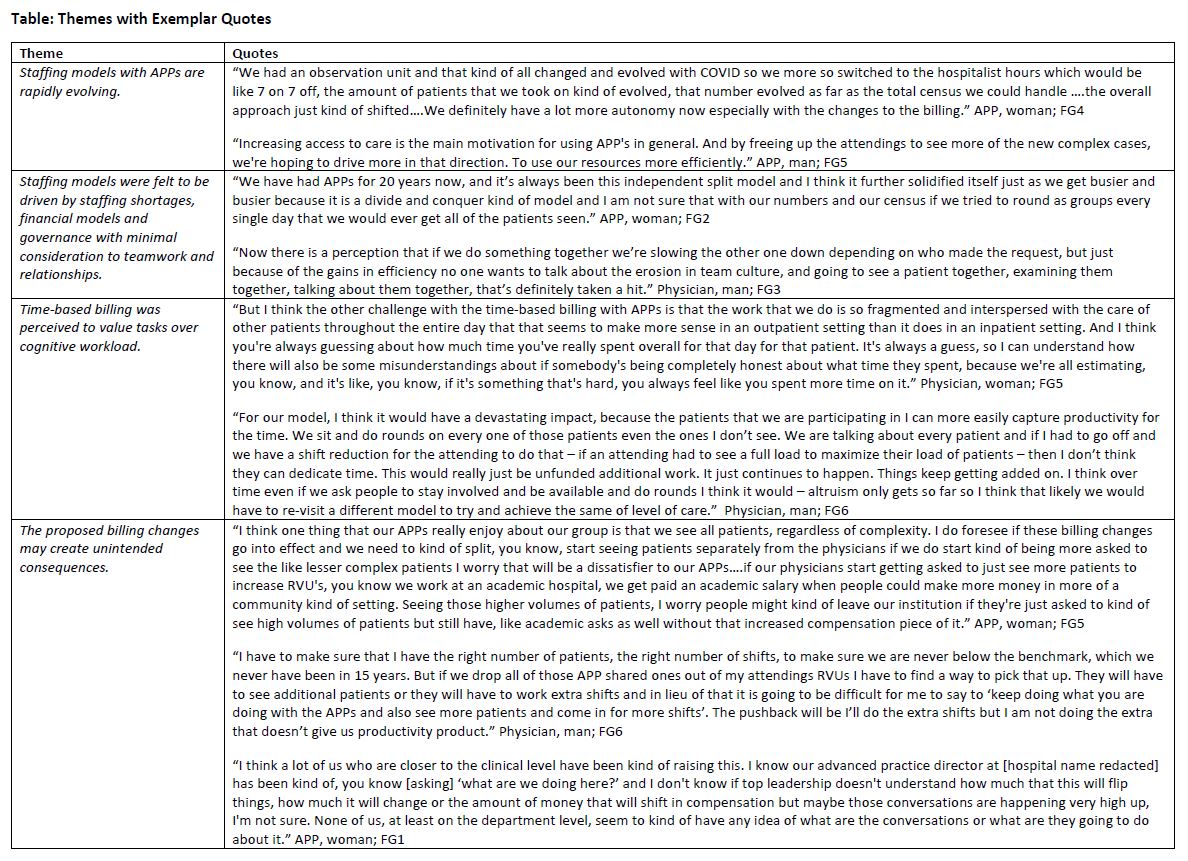
Results: Thirty-three individuals (physicians [n = 21], APPs [n = 10], practice manager [n = 1], and patient representative [n = 1]) participated in focus groups conducted via Zoom videoconferencing on March 20, 2023. Twenty-seven of the 33 individuals (81.8%) completed the survey. Participating hospitalist groups ranged in size from 28 to 125 physicians (mean 65.5, IQR 44.25-76.25) and zero to 70 APPs (mean 22.2, IQR 9.75-28.75). Fifteen participants (57.7%) responded that APPs bill independently, 17 participants (65.4%) responded that physicians and APPs bill shared services with the collaborating/supervising physician and three participants (11.5%) responded that APPs do not provide billable services. Four themes emerged from analysis of the focus groups: (1) Staffing models with APPs are rapidly evolving and include a variety of staffing models utilizing APPs in the care team. (2) These changes were driven by staffing shortages, financial models, and governance with minimal consideration given to teamwork and relationships. Participants described greater autonomy for APPs in response to surge demand from the pandemic that has persisted due to perceived cost and operational efficiencies; however greater independence has also led to less collaboration between physicians and APPs with the perception that independent models are seen as less safe. (3) Time-based billing models were perceived to value tasks over cognitive workload, and this may disincentivize physician involvement in care. (4) The proposed billing changes may create unintended consequences including dissatisfaction among both physicians and APPs as well as erosion of culture between physicians and APPs. See the Table for exemplar quotes.
Conclusions: Physician and APP collaborative care models are increasingly evolving to independent visits often driven by workloads, financial drivers, and local regulations such as medical staff rules and hospital bylaws. While CMS has now revised billing rules for split or shared visits to include either time or medical decision making, understanding which staffing models produce optimal patient, clinician and organizational outcomes is needed and should inform billing policies rather than the reverse.