Background: When the Accreditation Council for Graduate Medical Education established new regulations for resident work hours, this resulted in an increase in patient handoffs and discontinuity of care in residency training, necessitating resident rotations requiring night cross-cover.(1,2) The annual survey of clerkship directors in 2014 showed only 38.7% of students experience nights during their clerkship and 40.7% during their sub-internship.(3) A 2019 survey of interns across medical specialties showed most had no formal cross-cover training and felt unprepared to serve in this role.(4) To meet this training need, we developed a direct care hospitalist service (DCHS) sub-internship pairing hospitalists with sub-interns (sub-Is) with 1 week of direct night float cross-cover experience.
Purpose: We developed a dedicated cross-cover experience into the DCHS sub-internship experience. As part of the subinternship rotation, 1 of 4 weeks was night float cross-cover and admissions where sub-Is cross-cover up to 16 patients and admit 2 patients for 4-5 nights. We aimed to increase student comfort with emergencies and overnight clinical scenarios to prepare for cross-cover rotations during intern year.
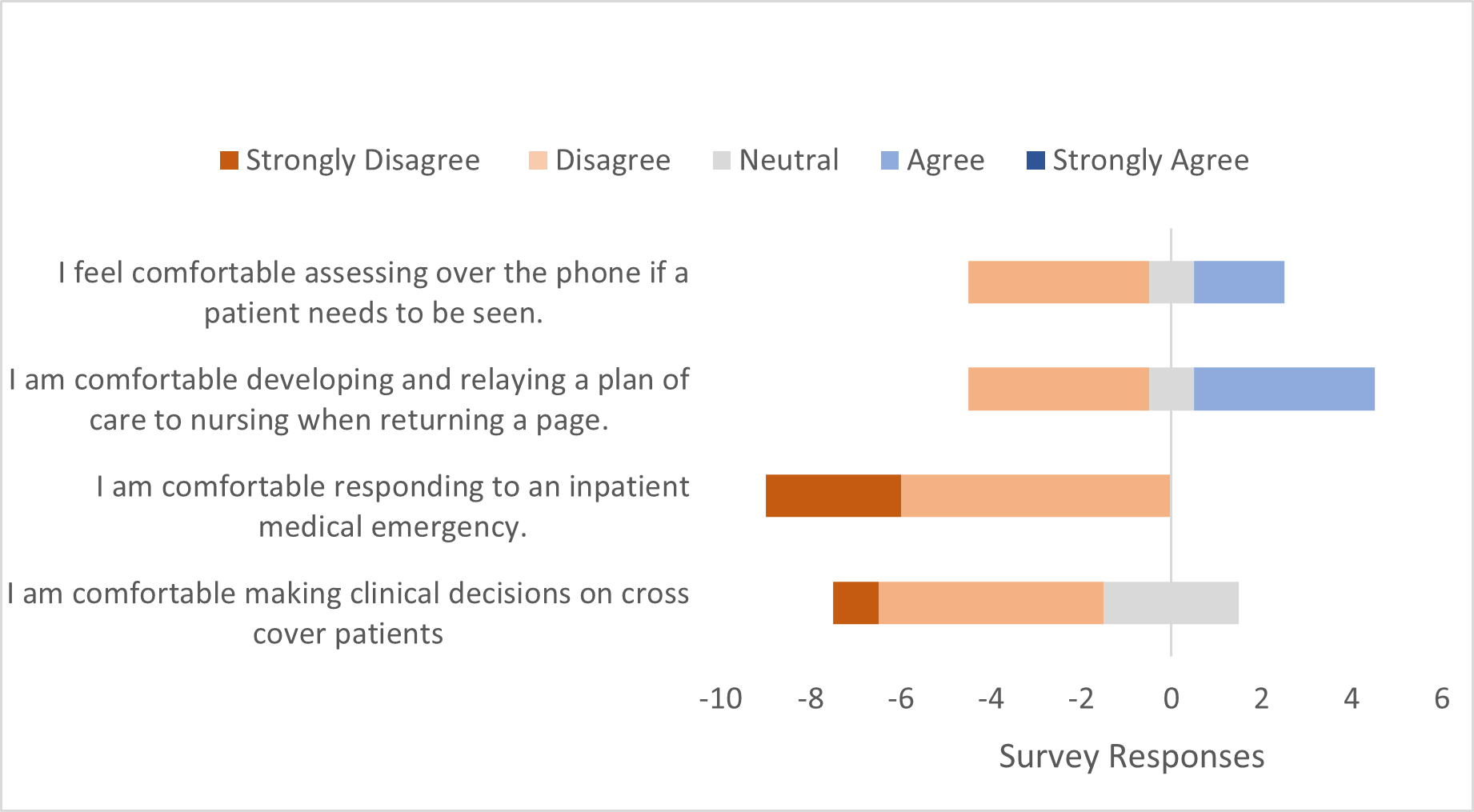
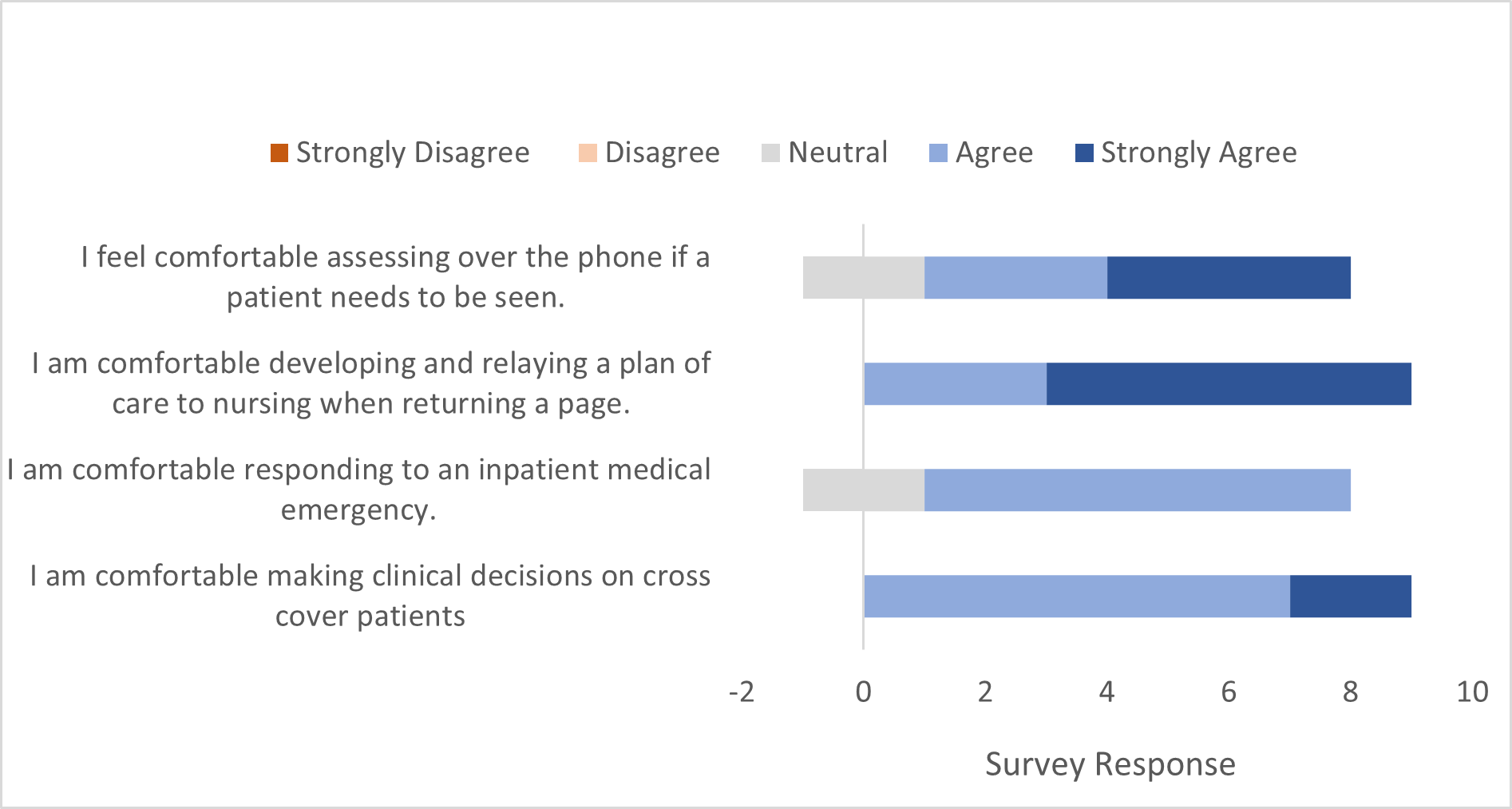
Description: From August to November 2023, we surveyed 9 fourth year medical students rotating through our night cross-cover experience using a REDCap survey. They completed 5 12-hour night shifts during their sub-internship. Students ranked their comfort using a 5-point Likert-type scale with 4 items related to cross-cover clinical skills: 1) relaying a plan of care; 2) responding to an emergency; 3) clinical assessment over the phone, and 4) making clinical decisions. Invitations to the survey were e-mailed to students after their night orientation prior to their first night and at the conclusion of their night block. One email reminder for the post-night survey completion was sent 7 days after the end of their rotation. Comparison was performed by paired t-test. Response rate was 100%. Students were more comfortable making clinical decisions on cross cover patients (mean 2.2, SD 0.67 pre and mean 4.2, SD 0.44 post, p 0.001), responding to an inpatient emergency (mean 1.7, SD 0.5 pre and mean 3.8, SD 0.44 post, p = < 0.001), and developing and relaying a plan of care to nursing overnight (mean 3, SD 0.33 pre and mean 4.7, SD 0.17 post, p 0.008) (Figures 1 and 2). The students felt more comfortable assessing over the phone if a patient needed to be seen (mean 2.8, SD 0.28 pre and mean 4.2, SD 0.83 post, p 0.08).
Conclusions: Most students feel uncomfortable with cross-cover even as late as their final year of medical school. This can lead to trepidation when students are asked to perform normal cross-cover tasks. With the inclusion of dedicated, supervised clinical training, the students completed the rotation feeling significantly more comfortable with all aspects of night cross-cover emphasizing the importance of dedicated cross-cover included in all medical curricula. While the results were not statistically significant, the students still did on average feel more comfortable triaging patients’ needs over the phone at the culmination of the rotation. Our next steps are to integrate rapid response simulations into the sub-internship and to assess clinical performance in intern year for students who had exposure to cross-cover training prior to starting intern year.