Background: Risk assessment for venous thromboembolism (VTE) is a part of every hospital admission. The workflow of who completes the assessment varies between hospitals, but often it is carried out by trainees. VTE risk assessment is further complicated by the variety of methods to identify those patients who are appropriate for chemoprophylaxis, mechanical prophylaxis, or no intervention. Understanding trainees’ knowledge of VTE risk stratification is important to provide directed education and to potentially modify their workflow to better align practice with guidelines. The purpose of this study is to evaluate Internal Medicine residents’ ability to appropriately risk stratify and recommend appropriate interventions for VTE prevention, in order to develop a directed educational intervention.
Methods: The study was conducted within an Internal Medicine residency at a ~300 bed, urban, community hospital. A survey of 10 case scenarios was created for respondents to classify the level of VTE risk (high or low), if there were contraindications to chemoprophylaxis, would they use chemoprophylaxis and if so what agent, and would they use mechanical prophylaxis. Each case also provided the opportunity to provide a brief free text explanation of their choices. The cases were all loosely based on actual clinical scenarios and selected to highlight specific knowledge areas related to appropriate VTE risk stratification. The surveys were administered to all residents present during a standard noon conference. Following the survey, a brief didactic session was given to go through the recommendations for each case. Each case was compared to a key created by the authors using the Padua score as a reference for medical patients and Caprini score for surgical (1), which are the preferred tools within the hospital electronic health record. In all cases with indications for chemoprophylaxis, there were no contraindications for enoxaparin, and therefore was designated the preferred agent (2).
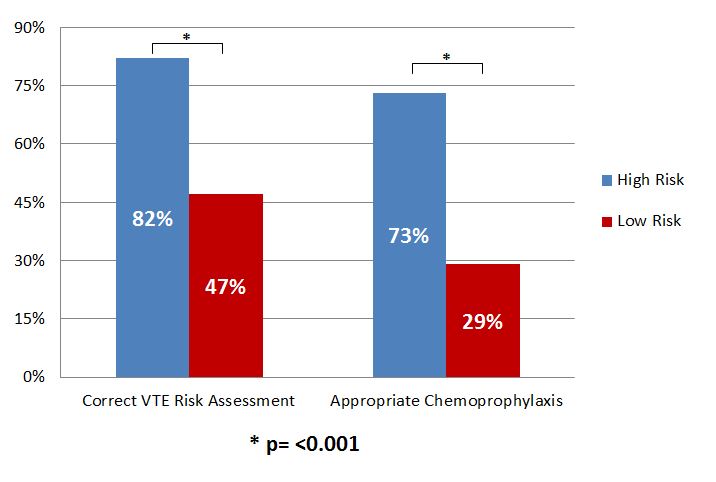
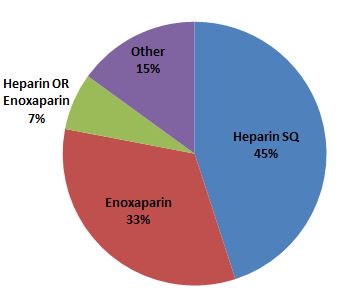
Results: A total of 30 residents (15 PGY-1s, 8 PGY-2s, 7 PGY-3s) were present at the conference and completed risk assessments on the 10 cases. Overall, 68% of the responses for VTE risk level were correct and 57% of the recommendations for chemoprophylaxis were appropriate. Between PGY-1 and PGY-2&3 residents, there was no significant difference in the proportion of correct responses for either risk (p = 1.0) or chemoprophylaxis (p = 0.3). Respondents were significantly more likely to correctly identify high risk compared with low risk medical patients and recommend appropriate use of chemoprophylaxis (Figure 1). When chemoprophylaxis was appropriately recommended, enoxaparin alone was chosen only 33% (Figure 2). In the single surgical case, chemoprophylaxis was correct for 90%, but only 10% appropriately recommended mechanical prophylaxis.
Conclusions: In the study population, Internal Medicine residents poorly acknowledged cases with low VTE risk and infrequently recommended appropriate chemoprophylaxis in those cases. Level of training did not impact accuracy of VTE risk assessment or chemoprophylaxis choice. The preferred chemoprophylaxis medication varied amongst respondents. Overall, future educational interventions will focus on identifying low VTE risk medication patients and consistently use enoxaparin as first line chemoprophylaxis when appropriate.