Background: Hematopoietic stem cell transplantation (HSCT) can be a life-saving and curative therapy in hematological malignancies. Pre-transplant evaluation for HSCT is a multidisciplinary process that can be complicated, time-consuming, and expensive for patients to navigate. The process requires coordination between several medical subspecialties including pulmonary, cardiology, and mental health, in addition to social workers and patients’ families. There is often a narrow window between achieving disease control and preserving performance status in order to receive a transplant. Thus, timely completion of pretransplant evaluation can be vital, as it can affect transplant outcomes and patient mortality. Within the VA medical system, there are three national centers for HSCT, which requires additional multi-center coordination. Our goal was to evaluate the HSCT evaluation process at our VA Medical Center to determine which elements required the most time and effort. We planned to reduce time to transplant in days by 25% for HSCT candidates over two years, from March 2018 to March 2020.
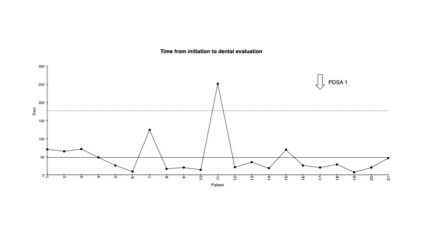
Methods: We reviewed data for 49 patients who underwent evaluation for HSCT from 2009-2019. We recorded the time from initiation of transplant evaluation to its completion. We also included time required to obtain studies such as pulmonary function tests (PFT) and transthoracic echocardiogram, as well as dental, mental health, and psychosocial consultant evaluation. A process map (attached) and fishbone diagram revealed several barriers and time-consuming steps. We used Lean Six Sigma principles to learn that the lack of a formal clinic and navigation process were a main source of waste and inefficiency.The interventions performed during the first PDSA cycle included a formal HSCT consult order and clinic appointment, a Telemedicine clinic appointment with national transplant centers, and the hiring of additional mid-level providers to help coordinate evaluation. The second PDSA cycle included an order set for both required lab workup and consult orders, reviewing with subspecialty departments such as cardiology and pulmonary to ensure the most effective means to obtain TTEs and PFTs, respectively, and a printed handout for patients. We used XmR statistical process control charts to evaluate the effect of these interventions. IRB was obtained per institutional protocol.
Results: Our baseline process analysis revealed that the psychosocial evaluation, mental health referral, and dental referral took the longest time during HSCT evaluation. After the first PDSA cycle, the average time to HSCT referral improved from 101.9 days to 94.5 days. Patients had improved time from referral placement to completion of dental evaluation, PFTs, and mental health evaluation (XmR chart for dental consult attached). Data collection from the second PDSA cycle is ongoing.
Conclusions: Referral for HSCT requires a complex decision-making process with hematology expertise, multidisciplinary evaluation, and interfacility care coordination. At our medical center, the implementation of a formal HSCT evaluation order set, dedicated clinic, and patient education helped reduce dependency on providers for consistent follow-up. Areas for future improvement include a potential formal social work consult and a weekly HSCT team coordinator meeting. There was a tremendous effort on behalf of caregivers to improve patient navigation through this difficult process, which was greatly appreciated.