Background:
Pneumonia readmission rates are publicly reported and included as quality indicators in Medicare Value-Based Purchasing programs. The Yale New Haven Readmission Risk Score (YNHRRS) for Pneumonia is a tool that uses 25 variables including age, co-morbidities, and vital signs to predict readmission. Functional status and social support were not included in the YNHRRS, despite evidence that they affect readmission rates. Because the original tool was validated in a cohort of Medicare patients, we sought to investigate its generalizability by applying it to all patients with pneumonia. In addition, we extended the tool to assess functional status (FS) and social support (SS) to determine whether these factors strengthened its predictive value.
Methods:
We performed a retrospective chart review for all patients hospitalized at an academic medical center between March 2014 and March 2015 with a primary diagnosis of pneumonia. The 25 variables of the YNHRRS model were abstracted and the YNHRRS was calculated for each subject using the model coefficients from the original study. Data regarding FS and SS were extracted from the admission database, in which nurses recorded information about patients’ need for assistance with walking, getting out of bed, feeding, grooming, or dressing, and if they had someone at home to assist with medical care.
Our primary outcome was 30-day readmissions. We fit a logistic regression model to predict readmission using the YNHRRS, FS and SS assessments as covariates. In addition, we calculated the area under the receiver operating characteristic curve (AUC) for the model.
Results:
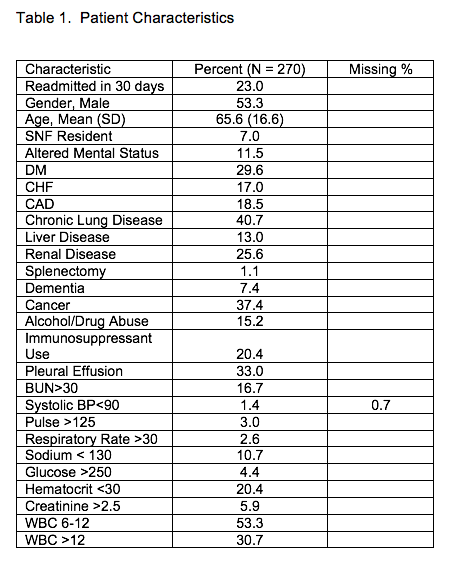
270 subjects with pneumonia were admitted during the study period. Patients had a mean age of 65.6 (SD 16.6), 53.3% were men, and the rate of readmission was 23.0% (Table 1). The YNHRRS was a significant predictor of readmission (OR 2.20 [95% CI 1.29-3.73] for each 10% increase in calculated risk, (p=0.004) in our multivariate model. Non-significant predictors included nursing assessments of need for help walking (OR 0.85 [95% CI 0.34-2.09], p=0.72), need for help with activities of daily living (OR 1.25 [95% CI 0.44-3.51], p=0.68) and presence of social support (OR 0.67 [95% CI 0.37-1.21], p=0.18. The AUC of the model was 0.60.
Conclusions:
The YNHRRS performed comparably to the derivation study as a predictor of readmissions in an unselected cohort of pneumonia patients. Markers of FS and SS were not significant predictors when added to the YNHRRS. This is the first study we are aware of that demonstrates the validity of a pneumonia readmission risk tool in a general hospital population. Better indicators of FS or strength of SS may exist, so our inability to show a linkage to readmissions should not preclude further investigation.