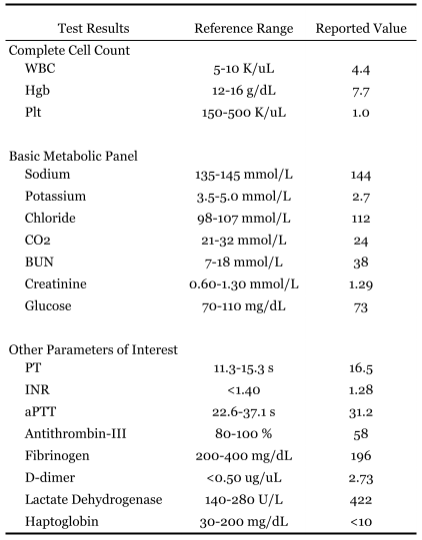
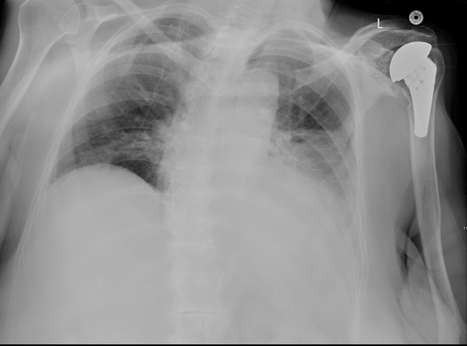
Case Presentation: A 84-year-old woman with a past medical history of HTN, DM2, CHF, and hypothyroidism presented to an offsite ED after falling on her buttock when rising from a kitchen chair. She had an uneventful course of COVID-19 four weeks prior. Over the last 2 weeks, she developed progressive weakness. Upon arrival at the ED, the patient could no longer ambulate independently.There, she was tachycardic and hypotensive, and her CT head showed no acute abnormality. Her CBC revealed anemia (Hgb 6.8 g/dL) with severe thrombocytopenia (2.0 K/uL). Additionally, her CMP revealed an elevated creatinine (1.9 mmol/L) and elevated bilirubin (4.1 mg/dL). She was transfused with 1-unit of PRBCs and 1-unit of platelets before being transferred to our facility.At our facility, the patient’s vitals were stable. She was A&Ox3 and denied other complaints. Her physical exam was notable for a large contusion to the buttock with multiple ecchymoses. Lab workup revealed anemia with thrombocytopenia, as well as decreased antithrombin-III, decreased fibrinogen, elevated lactate dehydrogenase, low haptoglobin, and elevated D-dimer (Table 1). Hematology was promptly consulted. Concern was raised for immune-mediated hemolysis, and patient was promptly started on 125 mg of methylprednisolone every 12 hours.For seven days, the patient’s cognition was unchanged from baseline, and her vitals were within normal limits; however, her condition remained guarded as a slow uptrend was observed in her cell counts. Blood smear and bone marrow biopsy results ruled out myelodysplastic process, implicating Evans syndrome, a rare condition characterized by the combination of autoimmune hemolytic anemia (AIHA) and immune thrombocytopenic purpura (ITP).On hospital day 8, the patient’s mentation and respiratory status acutely decompensated. CT head revealed no acute abnormalities. Chest x-ray revealed a new wedge-shaped alveolar opacification in the left-lower zone (Figure 1). She remained in critical condition until passing away that evening.
Discussion: Evans syndrome is a rare immune-mediated condition resulting in the combination of AIHA and ITP [3]. Moreover, cytopenias observed in Evans syndrome are often reported to be more severe than those seen in either AIHA or ITP alone. [1,2] In those older than 60-years-old, the prognosis is grim as there is an increased risk for ACS, PE, or CVA. As is the case with all other immune-mediated cytopenias, established evidence-based therapy does not exist. (4,5) Early introduction of corticosteroids is considered the first-line recommendation with Intravenous immunoglobulin therapy being in conjunction or alone. (4,6)With Up to 50% of Evans syndrome cases being secondary to immune dysregulation, the COVID-19 pandemic, gives clinicians further challenges in dealing with autoimmune cytopenias triggered by SARS-CoV-2 infection. [8,9] Reports of autoimmune cytopenias secondary to COVID-19 beyond those limited to Evans syndrome have also been reported.
Conclusions: Herein, a case of Evans syndrome thought to be secondary to COVID-19 is described. Despite gold standard management with corticosteroids, the reported patient succumbed to acute exacerbation. As a disease process involving immune dysregulation, COVID-19 can trigger immune-mediated cytopenias, such as Evans syndrome; therefore, in the midst of the ongoing global health issue, this report aims to highlight a unique sequela and its management.