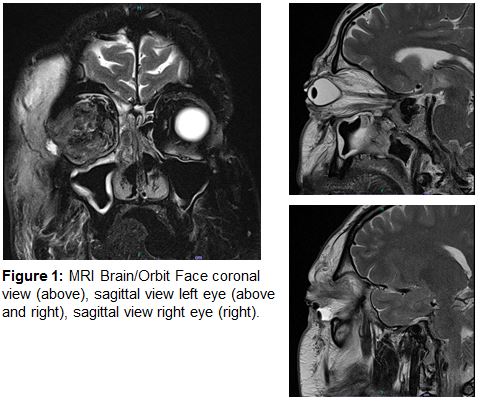
Case Presentation: Patient is a 41-year-old male with no relevant medical history who presented with 3 days of right orbital swelling. Accompanying symptoms included fevers, chills, and tinnitus. There was erythema above the right vermillion border with extension to the nasal cavity and right orbit. Sensation to light touch was decreased over the V2 nerve distribution. Relevant labs included white blood cell count (12.1), ESR (15), and CRP (17.8). Initial CT of the orbits showed preseptal cellulitis with proptosis of the right globe without abscess. Patient underwent right nasal endoscopy followed by right orbitotomy. Intraoperative cultures grew Apophysomyces elegans. Treatment included liposomal amphotericin B and posaconazole for four weeks, and he was discharged on isavuconazole monotherapy.
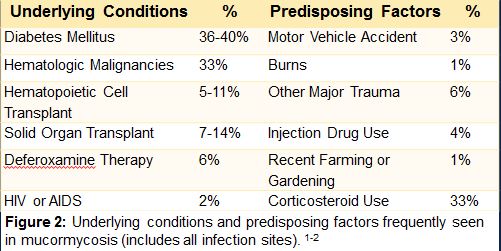
Discussion: Mucormycosis infections are caused by fungi in the order Mucorales, and are categorized based on anatomic location. Approximately 27 species within Mucorales are associated with human infection, with the Rhizopus genus being most common.1-4 Our patient developed rhinocerebral mucormycosis from Apophysomyces elegans, which is the fifth most common pathogen and accounts for approximately 6% of cases worldwide.2,3 Apophysomyces organisms can be found in North America, South America, Asia, and Australia.3 Within the United States, cases of mucormycosis caused by A. elegans are most commonly reported in southern states, such as Texas, Arizona, and Florida.5 Recently, the worldwide incidence of mucormycosis has increased, culminating in India’s announcement of a mucormycosis epidemic in May, 2021. Many have attributed the increased incidence to widespread corticosteroid use for the treatment of COVID-19, suggesting that selective use of corticosteroids in COVID-19 patients could limit mucormycosis incidence.15-17 Case reviews suggest that as many as 18-19% of mucormycosis infections occur in patients without underlying conditions.2,3 Common underlying conditions include diabetes mellitus, hematologic malignancies, hematopoietic cell transplantation, solid organ transplantation, treatment with deferoxamine, iron overload, HIV/AIDS, and corticosteroid use. Common mechanisms of infection include major trauma, burns, injection drug use, farming, or gardening.3,9 Ten days prior to presentation, our patient performed extensive yard work outside his Arizona home, which was likely the mechanism for his infection. He was otherwise devoid of risk factors (i.e. – normal fasting blood sugars, HIV screen, ANCA panel, immunoglobulin levels, lymphocyte subset panel, iron, and neutrophil function testing).
Conclusions: A. elegans is becoming notorious for causing mucormycosis in immunocompetent patients without underlying conditions.8-10 Recent literature suggests those infected with A. elegans are less likely to have an identifiable underlying condition, including a recent review that found 14 of 16 patients with A. elegans did not have any identifiable risk factors.19 It is still unclear which characteristics of A. elegans might contribute to its ability to infect immunocompetent hosts. In daily practice, providers in areas endemic to A. elegans should keep mucormycosis in their differential for immunocompetent patients with recent exposure to common mechanisms of mucormycosis infection such as farming, gardening, trauma, or injection drug use. Early recognition is imperative to ensure treatment with systemic antifungals, and surgical debridement.