Background: Interdisciplinary rounds are an important part of care coordination on medical units and on teaching units they usually are resident-led. After restructuring interdisciplinary rounds in our institution, we began including attending physicians, with the goal to improve care coordination, discharge planning and team communication.
Methods: The intervention was conducted on a 35-bed medical teaching unit at a tertiary care hospital. Starting January 2023, we involved our teaching attending physicians in interdisciplinary rounds, which previously included two resident teams, nursing (RN), case management (CM), physical therapy (PT) and pharmacy. Rounds remained resident-led, and attending physicians, now present in rounds, were asked to intervene if plan of care and discharge plan were not communicated accordingly. To assess our team member observations, we administered a yes/no survey as a screening tool and later implemented a Likert 5 point scale survey. The survey gathered team members’ opinions if attendings’ involvement improved clarity of discharge timing, discharge destination, and overall discharge planning, as well as clarity of medical plan and reduced errors in exchange of information. The surveys also evaluated teams’ opinion if patients’ and families’ discharge concerns were better addressed and if therapy services were utilized effectively. As objective measures, we compared length of stay (LOS), number of midnights and change in discharge timing before and after the intervention.
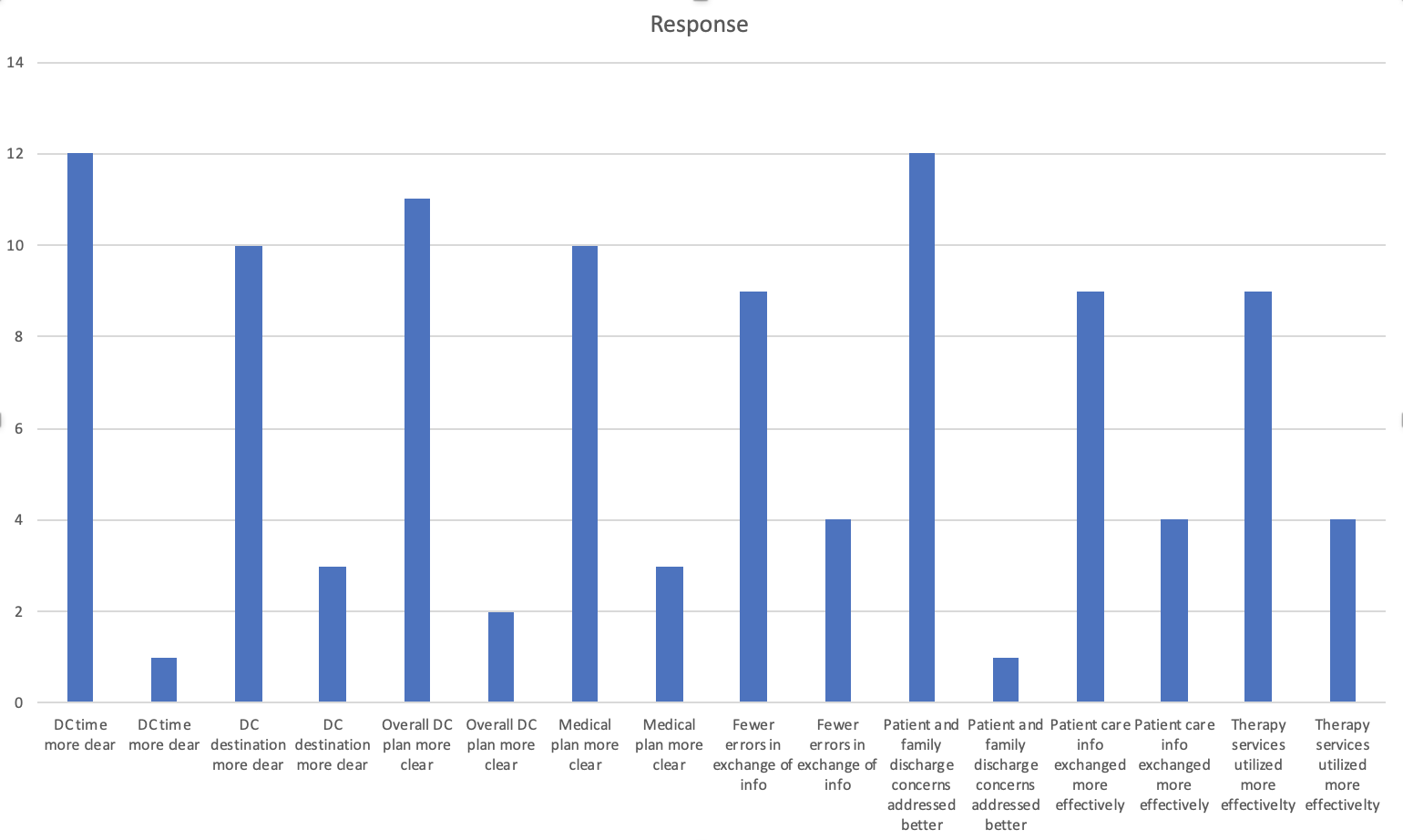
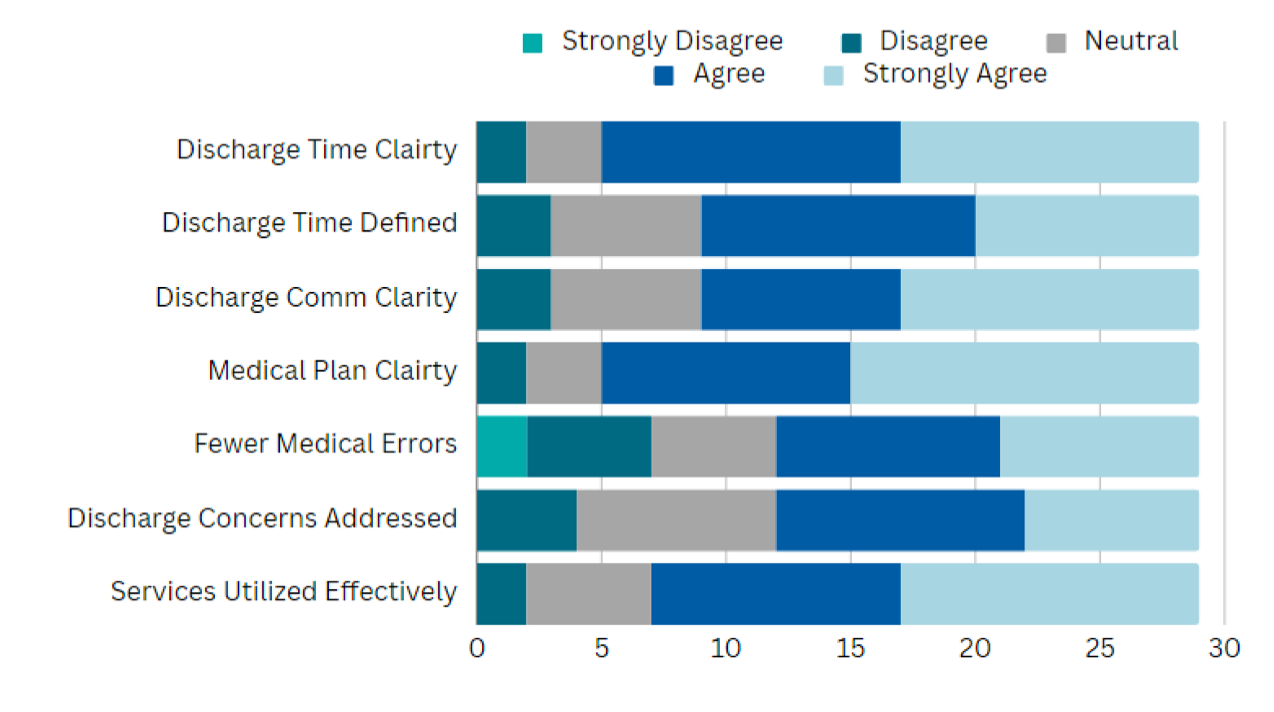
Results: We received survey responses from 42 team members, 13 with yes/no survey (figure 1) and 29 with Likert 5 point scale, as shown in figure 2 (17 RN, 3 PT, 9 CM, 8 resident physicians, 5 attending physicians). As shown in the figures 1 and 2, most of the team members felt improvement in discharge planning after attending physicians started participating in discharge rounds.LOS, number of midnights and discharge times were studied on a total of 3985 patients admitted to our unit, 1223 before the intervention (October – December 2022), and 2762 after the intervention (January – June 2023). 39 patients admitted in December 2022 and discharged in January 2023 were excluded. Student’s T-test showed significant reduction of mean LOS and number of midnights pre- and post-intervention. Pre-intervention mean LOS of 4.44 days was significantly reduced after the intervention to mean of 3.92 days (t(3969), p=0.00102, CI 0.21-0.82). Consistent with reduction of LOS – mean number of midnights was also significantly lower – from 4.65 to 4.09 days (t(3969), p= 0.00034, CI 0.25-0.87). There was no significant change noted in median discharge time using Chi Square test – median discharge time before the intervention was 15:57:05 and after the intervention 15:45 (p=0.95).
Conclusions: Including attending physicians in interdisciplinary rounds resulted in better clarity with the overall discharge planning as observed by team members and significantly improved length of stay in our unit, without affecting median discharge time. With growing complexity of our patients and ongoing challenges in navigating care coordination around hospital discharge, attending physicians participation in interdisciplinary rounds should be encouraged in order to achieve improved discharge planning and support of resident physicians.