Background: Balancing attending supervision with resident autonomy is intended to ensure patient safety while allowing trainees to gain graduated competency and independence upon completion of residency. ACGME work-hour restrictions have increased attending supervision, but its effect on resident education and autonomy is unclear. In order to better understand the underlying tensions and contributing factors to the culture of autonomy and supervision (A/S), we surveyed hospitalist attendings to explore their perspectives.
Methods: We created a 19-item web-based survey for all hospitalists at three inpatient sites of an urban academic medical center to explore perceptions and behaviors related to A/S. Questions included perception of the current and ideal culture of A/S, six unique clinical vignettes that assessed attending behaviors on a scale of “directly supervisory management” to “offered complete resident autonomy”, and free text responses eliciting hospitalists’ perspectives of, and suggested changes to, the current culture of A/S. We used descriptive statistics to summarize quantitative survey responses and content analysis to elucidate themes from free text comments.
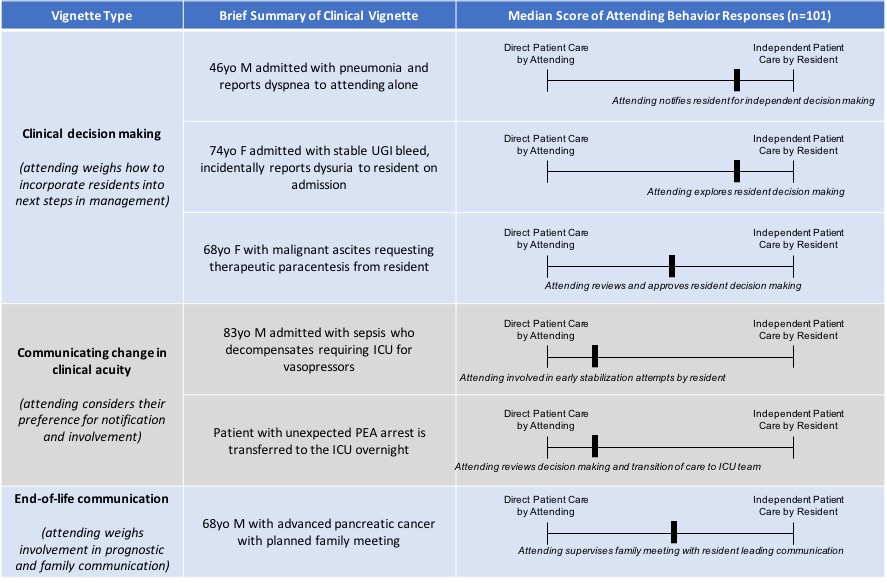
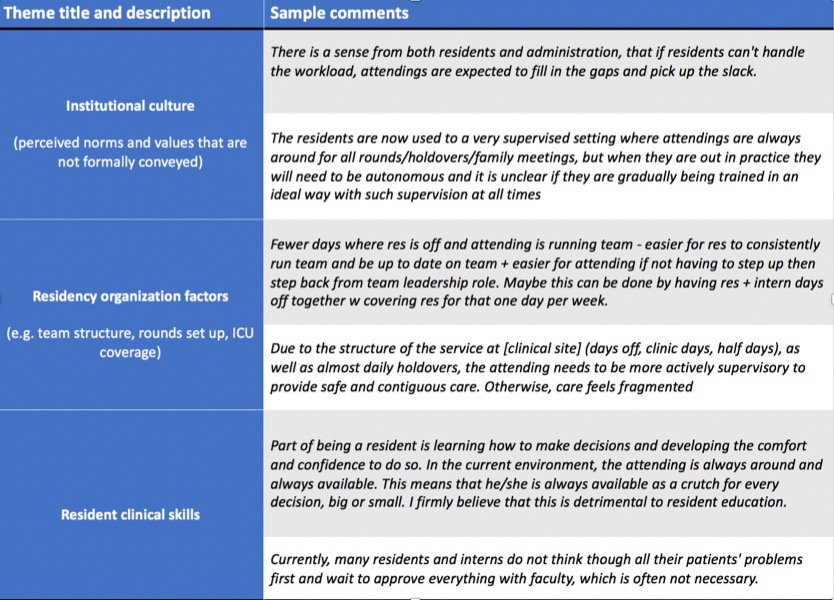
Results: Forty-nine percent of hospitalist attendings completed the full survey (101/206). On a scale of “entirely supervised (0)” to “entirely autonomous (100)”, hospitalists rated the average current culture of autonomy and supervision as 44/100, and the ideal culture as 59/100 (p<0.01). Forty-eight percent (n=57) of faculty described the culture of A/S they personally create to be equally autonomous and supervisory; 32% (n=38) more autonomous than supervisory; and 17.8% (n=21) as more supervisory than autonomous. Brief descriptions of the six clinical vignettes and hospitalist responses reflecting autonomous or supervisory behaviors are shown in Table 1. Hospitalists identified eighteen themes contributing to the gap between current and ideal culture, with the three most common being institutional culture, residency structure, and resident clinical skills (Table 2).
Conclusions: Our survey demonstrates a statistically significant difference between hospitalist attendings’ perceptions of the current culture of A/S compared to an ideal culture. Overall, the majority of vignette responses favor more resident autonomy in clinical decision-making, and trended towards more supervision during changes in acuity and end-of-life discussions. Additionally, results suggest that while hospitalists favor an ideal culture that is more autonomous than supervisory, they self-report that they create an equally supervisory/autonomous culture. Our study highlights the tension that hospitalists experience between the culture they desire to create and the barriers of perceived norms and current culture. Further studies are necessary to understand resident perceptions and competency-based outcomes related to the current A/S climate.