Background: Physician advocacy and knowledge of healthcare policy are vital elements of medical education and included within the ACGME Core Competency of Systems-Based Practice. The ability to advocate effectively has potential to impact healthcare regulations for both inpatient and outpatient practice. However, many GME programs do not incorporate these topics into their trainee education. To address this gap in our program, we introduced a resident curriculum on advocacy and healthcare policy. We administered surveys to determine knowledge and behaviors related to advocacy prior to the course, and to assess for changes following completion of the course.
Methods: All internal medicine residents at a single academic institution were invited to complete anonymous pre- and post-course surveys. Residents were surveyed on belief in the importance of advocacy, knowledge of healthcare policy, and participation in advocacy activities, using a 1-to-5 point Likert scale from “strongly disagree” to “strongly agree”. After the pre-survey, residents underwent a year-long curriculum of monthly lectures during morning conference on the US health insurance system, prescription drug pricing, social determinants of health, and legislative advocacy. Inpatient and outpatient topics were covered by an attending hospitalist with training in healthcare policy and advocacy. After completion of the lecture series, residents were re-administered the survey in June. Survey data was analyzed for changes pre- and post-course, as well as for differences by trainee gender and PGY level.
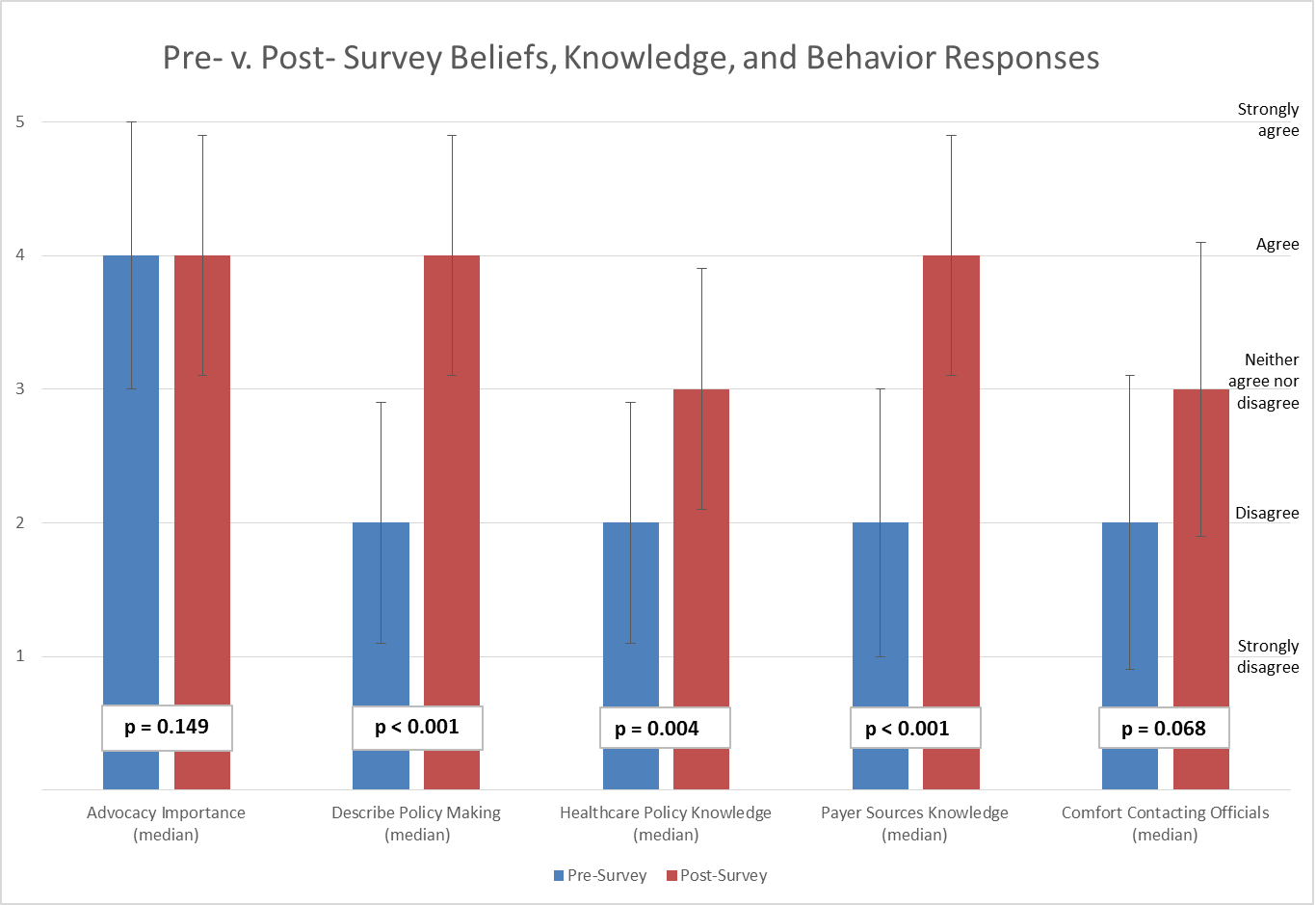
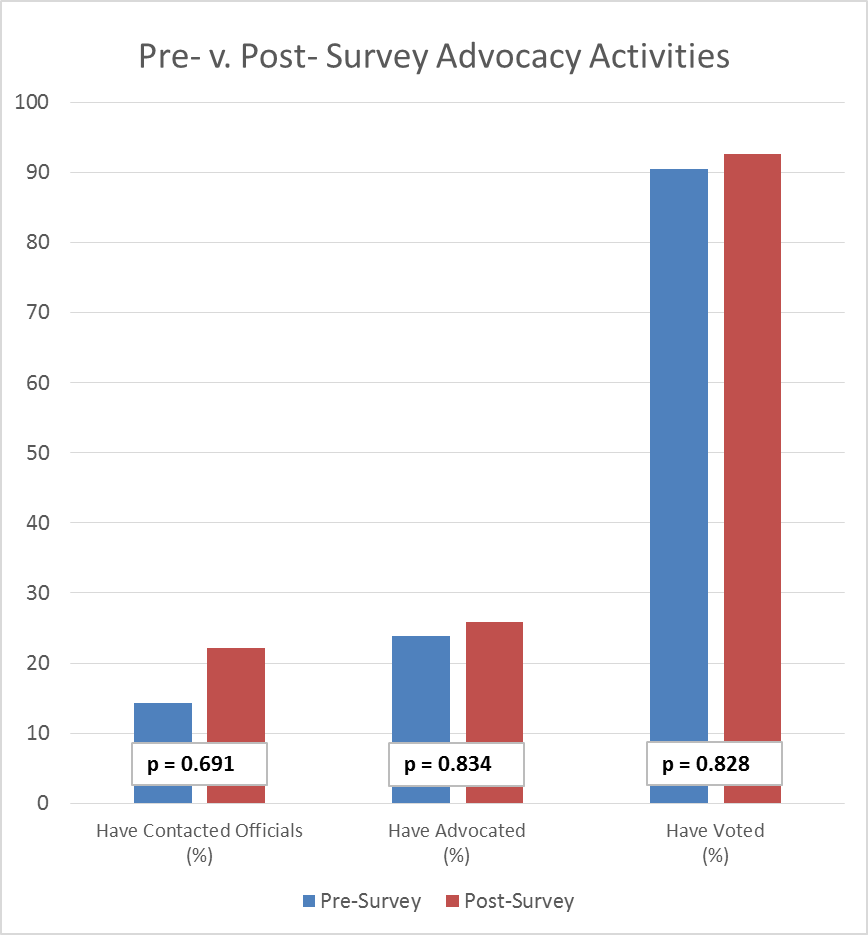
Results: All 47 internal medicine residents were invited to complete both anonymous online surveys. The pre-survey had 21 respondents (44.7%): 12 PGY-1, 9 PGY-2/3; 12 male, 9 female. The post-survey had 27 respondents (57.4%): 15 PGY-1, 12 PGY-2/3; 9 male, 16 female. See figures 1 and 2 for pre- vs. post-survey results. There were no significant differences by gender. Before the course, PGY-2/3s were more likely to report familiarity with current healthcare news compared to PGY-1s [Median±SD; 2.0±0.8 vs 1.0±0.9, p=0.041]. After the course, PGY-2/3s were more likely to report ability to describe policy making compared to PGY-1s [4.0±0.4 vs 3.0±1.0, p=0.005].
Conclusions: This study demonstrated the feasibility of administering a healthcare policy curriculum for internal medicine residents during scheduled conferences. Before the course, residents showed a discrepancy between having high levels of belief in the importance of physician advocacy, but low levels of both knowledge of healthcare policy and participation in advocacy. After the course, residents maintained high levels of belief in the importance of advocacy and showed increased levels of policy knowledge, but exhibited no change in behavior related to advocacy activities. This suggests that further interventions may be needed to promote resident participation in advocacy.