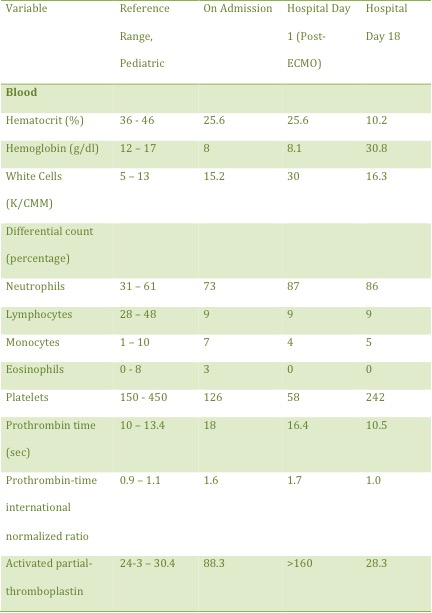
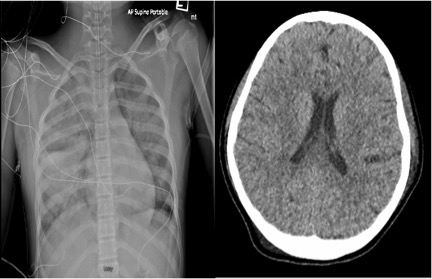
Case Presentation: We present a 12-year-old female with paresthesia and swelling to the left lower extremity. She was seen in the outpatient setting two weeks prior and diagnosed with cellulitis. After only two days of antibiotics, she presented to the Emergency Department for worsening symptoms; she was noted to have a blue, cold, and swollen left leg, which prompted further imaging. A duplex ultrasound revealed a large DVT, in the left internal iliac to popliteal. Vitals were: temperature 98.2oF, BP 135/76, HR 140bpm, RR 20, SpO2 99% on room air. The patient was in no acute distress but her left lower extremity was severely swollen, cool to the touch, erythematous and exquisitely tender. No palpable pulses were found, however a faint Doppler pulse was noted at the dorsalis pedis. The remainder of the physical exam was unremarkable. D-dimer was 1953 ng/ml (normal 130 mm/hr (reference range 0 – 13 mm/hr) and activated partial-thromboplastin time was 88.3 seconds. Fibrinogen was 191 mg/dl (reference 210 – 400 mg/dl). COVID-19 antibodies were positive. During thrombectomy she suffered a cardiac arrest during due to saddle pulmonary embolism (PE). CPR was immediately initiated. A bedside echocardiogram revealed hypokinetic and dilated right ventricle. After thirty minutes of CPR, a decision was made to place the patient on extracorporeal membrane oxygenation (ECMO), as she likely had a reversible cause of arrest. She was successfully placed on percutaneous VA-ECMO with subsequent return of spontaneous circulation. She subsequently underwent catheter directed thrombolysis (EKOS) for her PE with marked improvement of her right ventricular function on repeat echocardiogram. She was successfully de-cannulated and extubated with no neurological deficits despite prolonged down time. She also received catheter directed thrombolysis of her DVT after an inferior vena cava filter was placed. Discussion
Discussion: Phlegmasia Cerulea Dolens is a rare and serious disorder needing aggressive treatment. Being exceptionally rare, there have been only two documented cases of Phlegmasia Cerulea Dolens in the pediatric population. Patients with a diagnosis of Phegmasia Cerulea Dolens are at increased risk of morbidity and mortality even when appropriate treatments are rendered with complications such as limb ischemia, pulmonary embolism, and limb loss being cited in the literature.
Conclusions: The novel coronavirus has been rapidly progressing worldwide since it’s first recognition in 2019. Children to date have been minimally affected in the global pandemic, with children younger than 18 years accounting for less than 2% of all cases in the USA, with severe presentations and death due to COVID-19 among children being rare. Interestingly, some children presented with severe illness such as shock and multisystem inflammation, with overlapping features to Kawasaki Disease and Toxic Shock Syndrome termed pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS). To our knowledge, there have only been two documented cases in literature, of pediatric patients presenting with a DVT of such magnitude. As was seen in our patient, she did not have any respiratory features of COVID-19, but presented with classical DVT symptoms. Our patient had no predisposing risk factors for hypercoagulability; she presented with a life-threatening DVT likely secondary to COVID-19 and subsequent embolic phenomenon requiring VA-ECMO.