Background: The indications for lumbar puncture (LP) among febrile infants 29-60 days old continue to evolve. We studied febrile infants age 29-60 days with an ED visit and compared the characteristics and outcomes of those with and without an LP. We also describe the clinical course of infants receiving antibiotics before or after the LP.
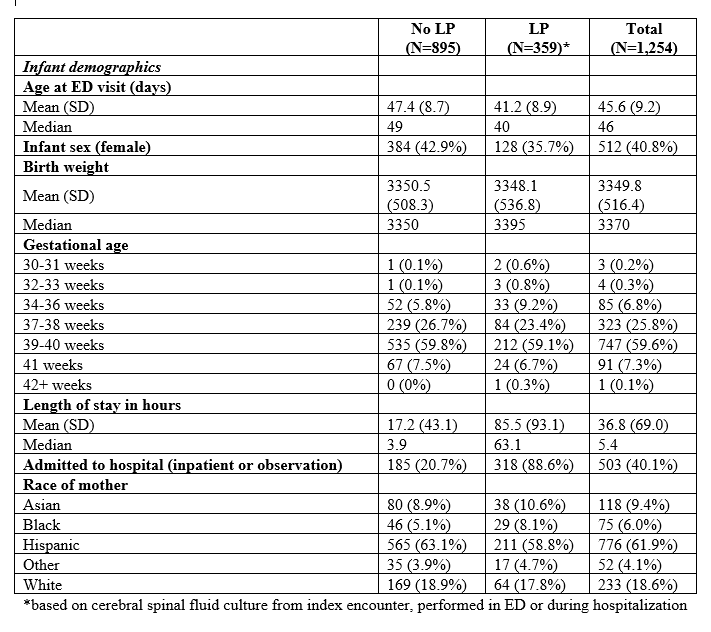
Methods: A retrospective observational study of febrile infants (29-60 days old) evaluated in one of 15 emergency departments (EDs) from January 2010 to December 2019. Study outcomes included culture positive meningitis, bacteremia, urine infection (UTI), respiratory virus results, 30-day mortality, receipt of successful LP (provider type), antibiotics, length of stay (LOS), hospitalization, and ED revisit or readmission within 30-days of encounter.
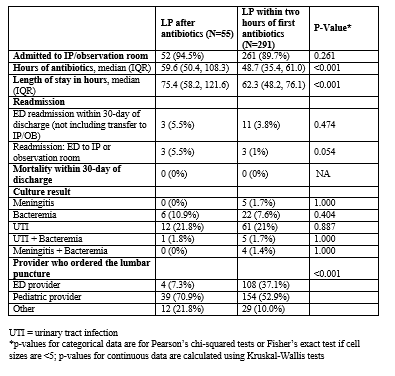
Results: We evaluated 1,254 febrile infants 29-60 days of age that presented to a study ED: 359 (28.6%) had a successful LP performed, 5 (0.4%) had culture positive meningitis, 37 (3.0%) had bacteremia, 149 (11.9%) had a UTI, and none died within 30 days. Two hundred ninety-six (23.6%) had a virus isolated on a nasal swab (LP 41.4% vs. no LP 63.3%). Five hundred fifty-nine patients (44.6%) received intravenous antibiotics (LP 96.4% vs. no LP 23.4%) and 503 (40.1%) were admitted to the hospital (mean LOS: 36h; SD: 69h). Thirty-eight (3%) returned to the ED within 30 days and 9 (0.7%) of those were hospitalized.Among the 359 infants who had a successful LP, 291 (81%) received an LP before antibiotics, 55 (15.3%) were done > 2 hours after, and 13 (3.6%) did not receive antibiotics. Five (1.4%) infants had culture positive meningitis, and all had an LP before antibiotics. Of these five infants, four had bacteremia with the same organism. There was no significant difference in the percentage of patients with bacteremia (7.6% LP pre-antibiotics vs. 10.9% LP post-antibiotics; p=0.40) or UTIs (21.0% LP pre-antibiotics vs. 21.8% LP post-antibiotics; p=0.89) between the groups.ED providers performed 108 (37.1%) of the LPs done before antibiotics and 4 (7.3%) of those done after. Pediatric providers performed 154 (52.9%) of those done before and 39 (70.9%) of those done after. The remaining 41 (11.8%) were performed by residents or primary care providers. Infants that had LPs performed after receiving antibiotics had longer LOS (median = 62.3h, [IQR: 48.2-76.1] pre-antibiotics vs. 75.4 [IQR: 58.2-121.6] post-antibiotics; p <0.001) and longer length of antibiotic use (48.7h, [IQR: 35.4-61.0] LP pre-antibiotics vs. 59.6 [IQR: 50.4-108.3] LP post-antibiotics; p = <0.001), but no difference in return visits to the ED (3.8% LP pre-antibiotics vs. 5.5% LP post-antibiotics; p = 0.474) or readmissions (1% LP pre-antibiotics vs. 5.5% LP post-antibiotics; p = 0.054). There were no deaths.
Conclusions: Our study found febrile infants 29-60 days old had favorable outcomes (no 30-day deaths, 1.4% culture positive meningitis) and most did not receive LPs (71.4%). Among those who received an LP, most (81.1%) were done prior to antibiotic administration. When LPs were done prior to antibiotics the LOS was significantly shorter, with similar patient outcomes. When ED physicians performed the LP, it was more likely to be done prior to receipt of antibiotics. Future efforts to optimize timing of antibiotics and LP completion may benefit patient care.