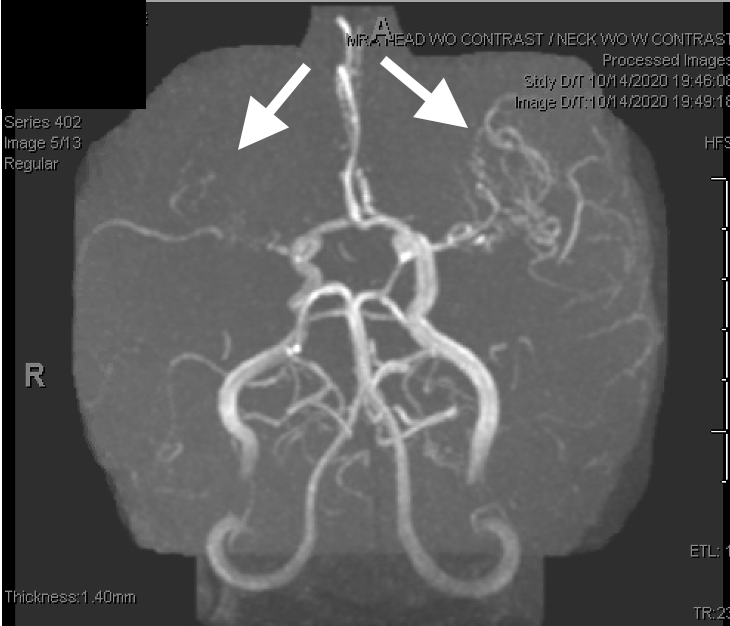
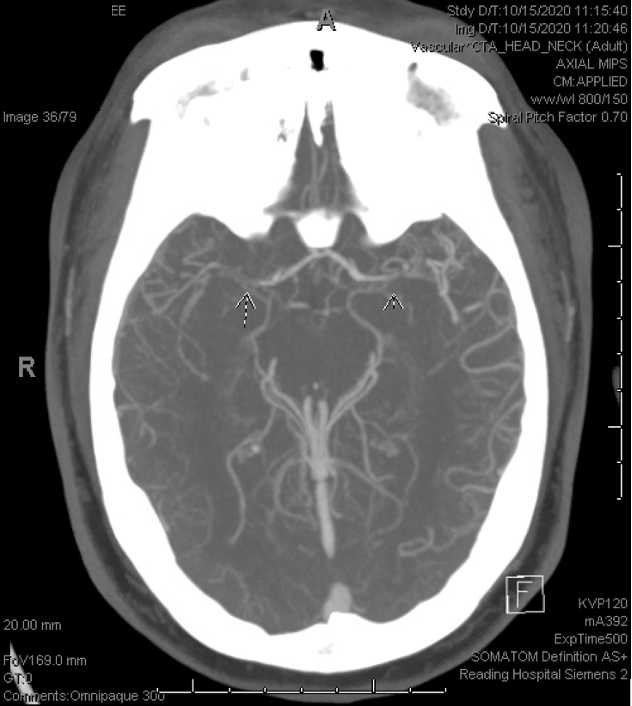
Case Presentation: A 28-year-old female with a history of recurrent deep venous thrombosis (DVT) on lifelong Xarelto, type 1 diabetes and iron deficiency anemia who presented with a recurrent acute DVT of the right lower extremity. During her hospitalization, she gave a history of intermittent left facial and right finger twitching that was self-resolving. These episodes had been occurring for several years, each incident several months apart, with reported recurrence of symptoms during the current hospitalization. She had been suspected of focal seizure-like activity due to these symptoms in the past, however reported persisting symptoms despite the use of carbamazepine for over a year. Routine EEG was unremarkable, lab values were within normal limits with the exception of elevated triglycerides at 601 mg/dl. Brain imaging was done with MRA, MRI, and CTA. MRI brain showed remote focal infarctions within the bilateral centrum semiovale. MRA showed an abnormal appearance of the M1 segments bilaterally consistent with a moyamoya pattern. CTA brain showed severe supraclinoid stenoses involving the ICA, ACA, and MCA vasculature in a pattern consistent with moyamoya (primary vs secondary). The patient was discharged on a high intensity statin and continued on her Xarelto. She was set up for an outpatient follow up with neurology for further investigational studies, such as catheter angiography, and likely surgical intervention.
Discussion: Moyamoya disease is a rare condition seen most often in patients of Asian descent, in children ages 5-10, and adults between 30-50 years old. Moyamoya can be primary due to a genetic mutation (moyamoya disease), or secondary to other underlying disorders, including Down syndrome, sickle cell anemia or neurofibromatosis type 1 (moyamoya syndrome). This disease is characterized by progressive stenosis of the carotid artery as it enters the base of the skull, with small collateral vessels forming over time to supply the brain distal to the area of stenosis, forming the characteristic “smokey” appearance on brain imaging. Common symptoms include stroke (ischemic and hemorrhagic), transient ischemic attacks, headache, visual disturbances, and developmental delay. In adults with this disease, intracranial hemorrhage is also seen, likely due to increased blood pressure and rupture of collateral vessels. However, some patients can present with more subtle findings such as fine, intermittent tremors of the hands which can be attributed to seizure-like activity.
Conclusions: Moyamoya is an uncommon disease with presenting symptoms that can be very subtle, or mistaken for individual disease processes such as stroke, seizure, or headaches. The etiology is often difficult to elucidate in younger individuals. There is no gold standard medical therapy for this disease, and many medications that would be used to symptomatically treat patients (such as antiplatelet therapy for suspected stroke or calcium channel blockers for headaches) could in fact put patients at increased risk for ischemic and hemorrhagic stroke. These potential risks outline the importance of keeping moyamoya in the differential for young patients presenting with symptoms suggestive of decreased or interrupted blood flow to the brain. Brain imaging with MRA and CTA for visualization of the cranial vasculature, along with catheter angiography and surgical revascularization, are imperative in preventing the morbidity and mortality that is inevitable with this progressive disease.