Background:
Effective patient‐physician communication is associated with improved patient experience and superior clinical outcomes. Designing interventions that have a measurable impact on physician communication scores, however, has been challenging. The aim of this study was to evaluate whether a physician identification tool used in an academic medical center would improve patient perceptions of physician communication, which prior studies have been unable to show.
Methods:
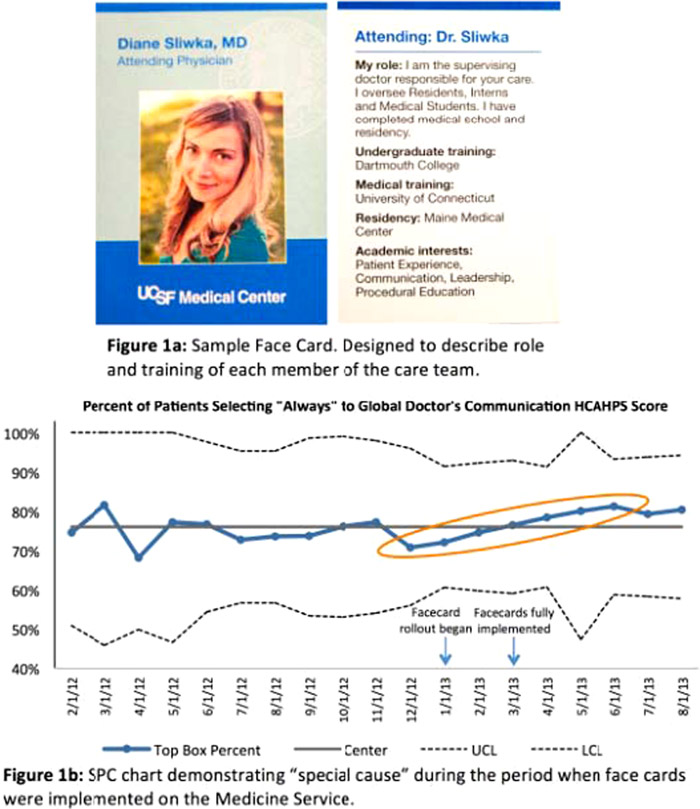
A physician identification tool, the face card, was designed and distributed to each Medicine resident and attending starting in January, 2013 (Figure 1a). Attendings received guidance on use of the card to introduce their name and role on the team, and were encouraged to model the behavior for residents. Thirty‐eight English speaking, cognitively intact medicine inpatients and forty‐three physicians participating in the first three months were surveyed regarding their experience. Responses from a patient survey, Hospital Consumer Assessment of Healthcare Provider and Systems (HCAHPS), regarding physician communication were obtained for February, 2012 to September, 2013. Top box scores were analyzed using statistical process control charts and compared to results for nursing communication from the same survey.
Results:
Of surveyed patients, 92% (35/38) wanted to receive a face card at future hospitalizations. 91% (39/43) of surveyed physicians agreed the face card enhanced introduction of team members, and 84% (36/43) agreed it did not disrupt workflow. Top Box HCAHPS scores regarding physician communication are shown in a statistical process control chart (Figure 1b), a methodology to differentiate if variation in a data set is attributed to a stable process, or if a special cause occurred to alter the system. A series of rules exist to detect special cause: in this case six upward trending data points, as indicated, identifies special cause correlating with our intervention. No trend was noted in survey responses regarding nursing communication during this same time period. There was no significant change in top box physician communication scores between the pre and post intervention period (74% versus 77%, p = 0.58). The annual cost to produce face cards for 200 physicians was $2800.
Conclusions:
Patient satisfaction is an increasingly important measure of high quality care, but it has been challenging to design interventions that demonstrably improve scores on physician communication. At our academic medical center implementation of physician face cards is feasible, low‐cost, and associated with improved patient perception of physician communication.