Background:
As the hospital workforce becomes increasingly interdisciplinary in recognition of the different skillsets required for effective patient care, high quality communication will become ever‐more critical. How often various team members communicate, and the paths along which information flows, is poorly understood. We used network analysis to document intra‐ and inter‐disciplinary communication in one hospital based on electronic communication.
Methods:
Our analysis relied on between‐provider communication using CareWeb Messenger (CWM), a system designed, developed, and implemented at our academic medical center as a web‐based, mobile‐enabled tool hybridizing Facebook and Twitter‐style functionality with text paging, treating each provider and patient as a “wall”. Users are able to view their own and patient’s “walls” but are able to message both users and non‐users on pagers or wireless phones. CWM tags each generated message by its sender/user, recipient, subject patient if applicable, and date/time, as well as the message’s content. We used the body of deidentified messages to visualize provider communication patterns using Gephi, an open‐source network visualization program.
Results:
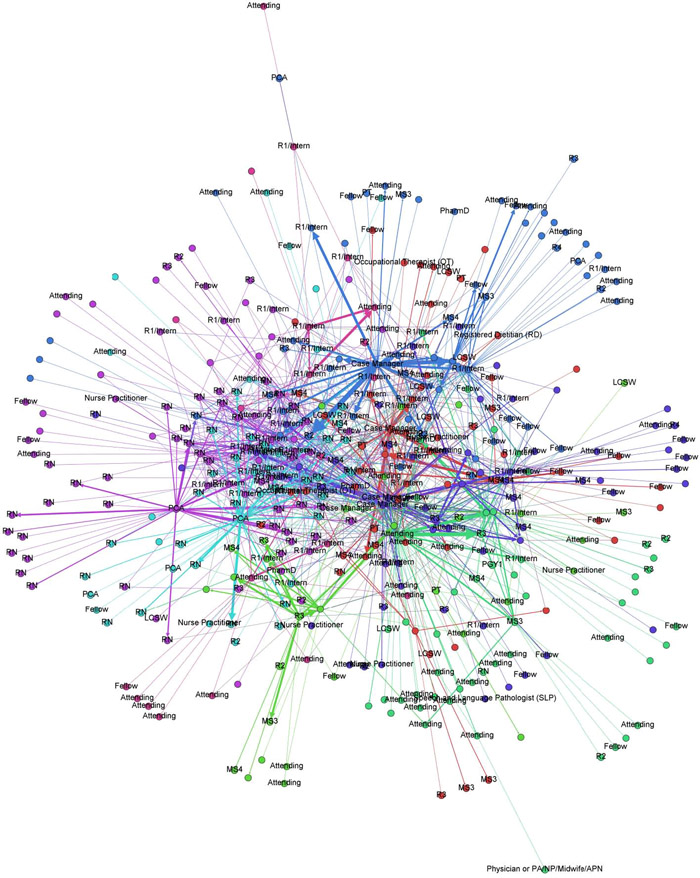
Between October 1 and November 13, 138 providers used CWM to send 4,062 message (2,589–64%–about specific patients), to 428 recipients. Case managers sent the most messages (178 per provider), followed by physicians (37) and nurses (33). Physicians received the most messages (61 per provider), followed by case managers (22) and nurses (20). In terms of users, interns (n=12) sent a mean of 23 messages each while attending physicians (n=8) sent a mean of 33 each. A network diagram is attached which illustrates all communication within the hospital by various providers of different disciplines; individuals placed closer together are more likely to have communicated with one another in the data that is sampled. The providers actively using the system represent a very small minority of the 8,000 employees at our medical center (less than 2%).
Conclusions:
In this preliminary, proof‐of‐concept analysis, we were able to plot inter‐ and intra‐disciplinary communication patterns in providers at our hospital who were using a new electronic communication tool. In the future, we foresee that such analysis could allow us to study the connectedness of various providers and disciplines to one another. We also plan to use these measures of connection and communication to assess correlation with outcomes such as length of stay and speed/appropriateness of response to clinical deterioration.