Background: With the rising predominance of shift work in healthcare, provider handoffs are important to facilitate the flow of patient information in a way that supports continuity and quality patient care. The Joint Commission has identified poor communication at handoffs as a major source of adverse events (1) which has led to significant work in standardizing nurse-to-nurse and physician-to-physician transitions of care (2-5). However, communication at shift change frequently does not directly occur between providers of different roles (6). Specifically, overnight bedside nurses do not typically hand off to daytime physicians creating risk of losing non-urgent patient information that may not have been deemed worthy of paging an overnight cross covering physician. As a regulatory requirement, nursing plan of care (POC) notes in our institution are completed at the end of each shift. However, with their existing template, the notes often do not include clinically relevant information. These nursing POC notes have the potential to facilitate communication of clinically relevant information from overnight nursing to daytime physician team.
Purpose: The aim of this project was to promote interdisciplinary communication and flow of patient information between overnight nurses and the daytime physician team. The intervention focused on adapting the nursing POC note format to include clinically relevant patient information and facilitate continuity of care.
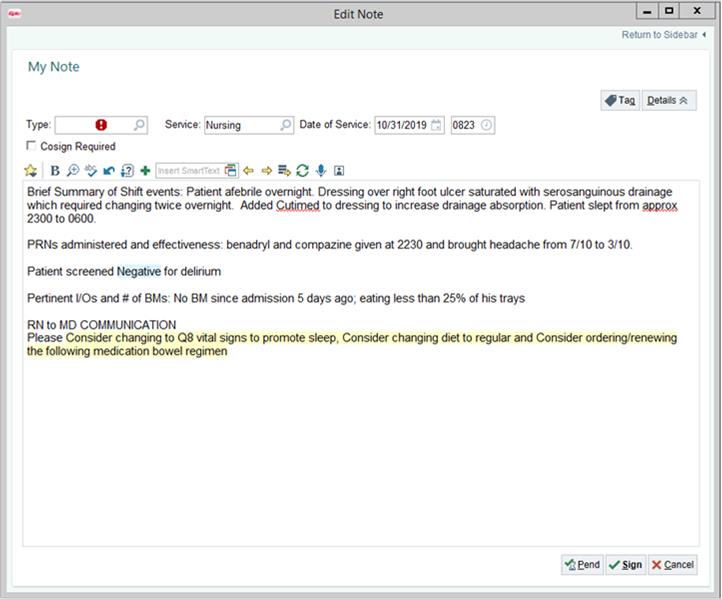
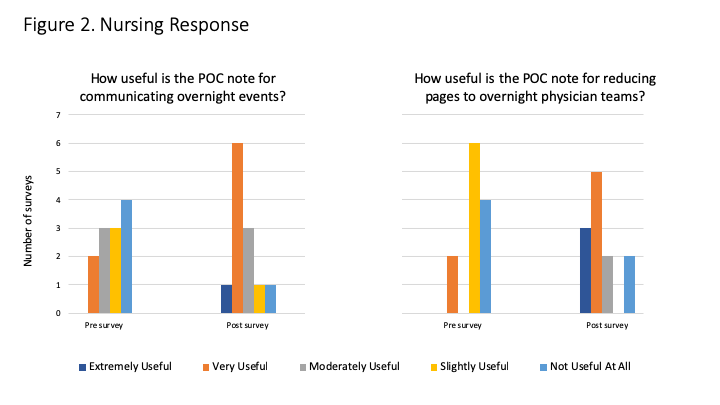
Description: A multidisciplinary group of nurses and physicians developed a SmartPhrase that was added to the standard nursing POC note, which included a brief summary of shift events, effectiveness of PRN medications, delirium screening, non-urgent communication (Figure 1). The note was implemented on a 26-bed acute care medicine unit for 10 weeks. Nurse and physician perceptions regarding impact on communication and patient care were assessed using qualitative surveys. Physicians were surveyed upon completion of rotation on the pilot unit and compared against a group of physicians on other medicine units as a control. Data was then collected from nurses on an additional 26 bed pilot unit in a matched, pre- and post-intervention assessment (n = 12). Regarding existing communication practices, night nurses on average felt they “rarely” communicate directly with the daytime physicians. In general, nurses felt the new POC note was more useful in communicating overnight events (p = 0.02) and in reducing pages to overnight physician teams (p = 0.004) (Figure 2). Nursing did not find a significant difference in the time to complete the new note. On evaluation of physician perceptions of the new POC note, there were statistically significant improvements in frequency that the note was reviewed (p = 0.02), communication of overnight events (p = 0.001), confidence that the note improved patient care (p = 0.001), comfort using the note as an alternative to paging (p = 0.01), and likelihood that the note was used to change care decisions (p = 0.002). Limitations of this initial pilot include the small number of nursing staff on surveyed units and lack of fully geographically aligned physician teams.
Conclusions: Overnight nurses often do not communicate with daytime physician teams. Implementing a standardized template with clinically relevant information in the nursing POC note may improve communication and flow of patient information between overnight nursing and daytime physician teams.