Background: Limited data exist about the magnitude of and the factors associated with one-year mortality of medical patients after their hospital discharge. Factors known during the hospitalization may be associated with high mortality risk. One may also wonder whether healthcare utilization during the first 30 days after discharge are also of any prognostic value for one-year mortality. We therefore aimed to identify factors associated with one-year mortality after hospital discharge, using data available at discharge, or 30-days after discharge separately.
Methods: This prospective, observational study included adult patients consecutively discharged to home or nursing home from the general internal medicine division of four mid-sized teaching hospitals in Switzerland. The primary outcome was all-cause mortality at one year after discharge collected by phone interview (patient, next of kin, or primary care physician [PCP]). Data from the index hospitalization were collected from the electronic health record and included demographic characteristics (age, gender, place of living, health insurance coverage), comorbidities, laboratory values (sodium, hemoglobin and albumin level at admission), assessment of nurse visits at home, distance to PCP, and the HOSPITAL score. Data at 30 days after discharge were collected by phone interview and included the number of emergency room and PCP visits, number of days of unplanned hospitalization after discharge and unplanned readmission were recorded. From variables available during hospitalization and for variables available 30 days after hospitalization, a univariable analysis was first performed, and additionally a multivariable analysis with one model using only data available at time of hospital discharge, and one model using data available after 30 days of discharge. The study was approved by the ethic committee at each participating site.
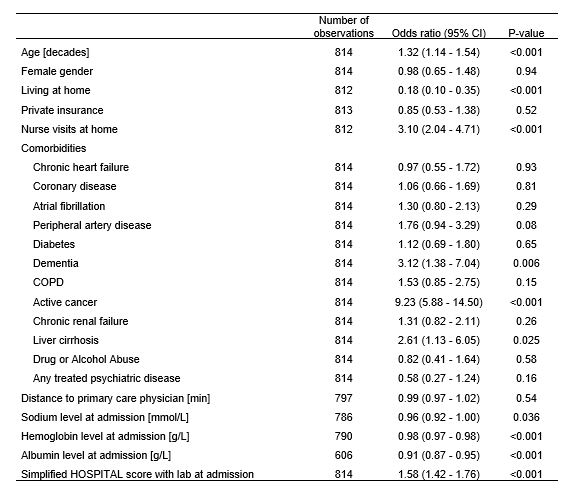
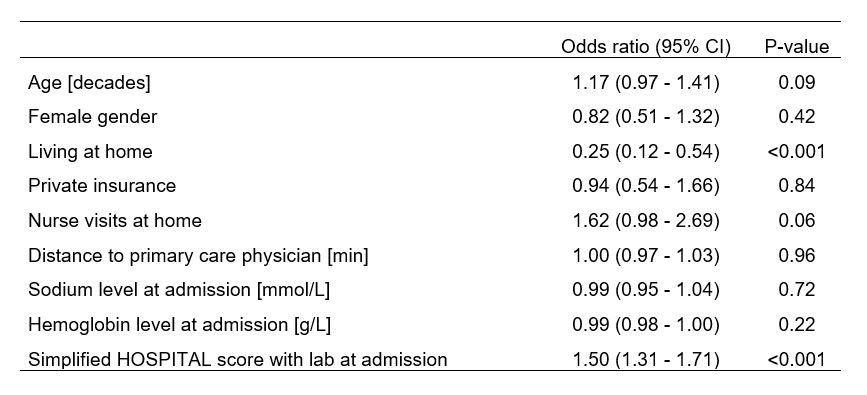
Results: Over the 9-month study period, 108 patients died out of the 814 with death status available (13.3%). The median age at time of discharge was 71 years (Interquartile range 58-80), and 44% were female (N=408). The effect of factors available at time of hospital discharge on one-year mortality are presented in Table 1 with odds ratio (OR) and 95% confidence interval (CI). The factors available 30-days after discharge associated with one-year mortality were any unplanned hospitalization (OR 5.84, 95% CI 3.65-9.36, p<0.001), and any emergency department visit (OR 2.94, 95%CI 1.70-5.11, p<0.001). Any PCP visit within 30 days after discharge had an OR of 0.63 (95%CI 0.38-1.03, p=0.07).In a multivariable logistic regression with factors available at discharge the simplified HOSPITAL score and living at home were predictors of one-year mortality (Table 2). In the multivariable analysis with predictors available at 30 days after discharge, only a 30-day unplanned readmission was significantly associated with one-year mortality (OR 4.81, 95%CI 2.77-8.33, p<0.001). A PCP visit within 30 days were negatively correlated without reaching statistical significance (OR 0.67, 95%CI 0.40-1.13, p=0.13).
Conclusions: The simplified HOSPITAL score predicted one-year mortality, which was higher in patients not living at home compared to those living at home. Different use of health-care within 30 days after discharge was associated with one-year mortality, i.e. mortality was higher in those with unplanned readmission and somewhat lower in those with a PCP visit.