Background: Sepsis, which is life-threatening organ dysfunction occurring in response to systemic infection, is a frequently fatal syndrome for which early recognition and treatment are paramount. While there are some reports that female and black patients with sepsis experience greater delays in time to antibiotics, there is an overall paucity of published data on whether there are disparities in the acute management of sepsis. The purpose of this study was to further investigate whether demographic factors were associated with time to antibiotic administration among patients with sepsis at our institution.
Methods: We obtained computerized electronic health record (EHR) data from all patients presenting to the Emergency Department (ED) at an 800 bed tertiary-care hospital between 6/1/2012 and 12/31/2016 for whom blood cultures were drawn within 72 hours (N=25,441). We limited our analysis to 9,006 patients who had 1) sepsis and 2) received intravenous (IV) antibiotics within the first 24 hours of presentation to the ED. EHR databases were queried to obtain data on patient demographics, discharge diagnosis codes, and sepsis criteria. Sepsis was defined as the presence of both of the following criteria: a Sequential Organ Failure Assessment (SOFA) score ≥2 within the first 24 hours, and ≥1 infections identified as a discharge diagnosis. The dates and times of antibiotic administration were obtained from pharmacy records. A multivariable linear regression analysis was performed to examine the association between time to first antibiotic and age, sex, race, primary language, diagnosis, and year.
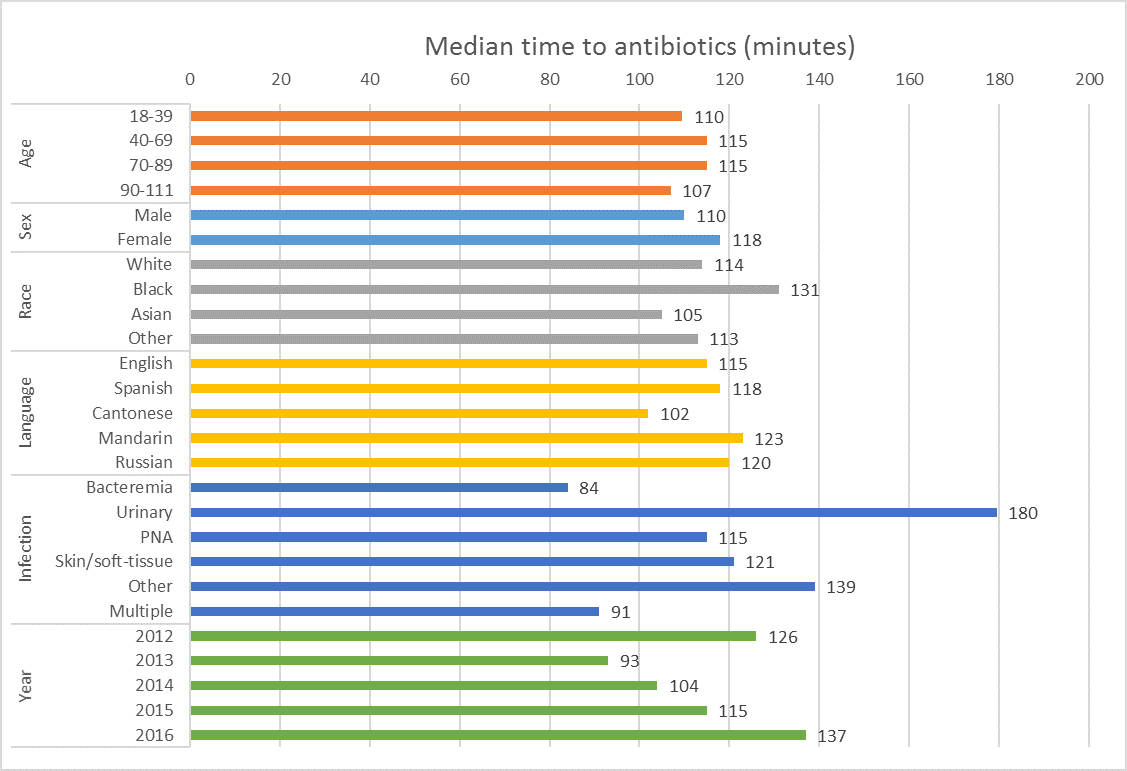
Results: Among 9,006 patients with sepsis treated with IV antibiotics within 24 hours of presentation, 5,912 (66%) had a single diagnosed site of infection at the time of discharge, while 3094 (34%) had more than 1 infected organ system. Most common single infections were pneumonia (21%), bacteremia (12%), and urinary tract infection (11%). The median time to antibiotics was 113 minutes. The percentage of patients treated with antibiotics at 60, 120, and 180 minutes was 29%, 52%, and 67%, respectively. The timing of antibiotic administration did not change significantly between years 2012 and 2016. Following multivariable adjustment, the only significant association with time to antibiotics was type of infection.
Conclusions: In this single-center hospital, we found no disparities in time to antibiotic administration by age, race, gender, or primary language, in contrast to some other published studies. Nearly 1/3 of patients with sepsis had not received antibiotics by three hours after presentation to the ED.