Background: Obtaining the Best Possible Medication History (BPMH) is the protocolized gold standard in obtaining medication histories and well known to decrease the total number of medication errors during transitions in care. Trained technicians require an average of 15-30 minutes to collect a BPMH [2]. Our facility conducted a categorical analysis and within subject study to determine which variables have the greatest influence on time to complete a medication reconciliation (MR) during admission. The data included information on patient demographics, the medium used to obtain the history, and the number of errors. Understanding which variables of MR collection have the greatest influence on the amount of time to obtain may be valuable when searching for more cost effective and safety driven methods of practice.
Methods: The BPMH was obtained on 817 adult patients over a seven-week period. Variables collected from each interaction include: participant ID, day of the week, age, gender, time taken, ethnicity, race, primary insurance, in-network patients, admitted from, previous admission, previous med history, English speaking, medication assistance, advanced sources (External Health Records, Prescription Monitoring Plans, etc.), medication list/bottles, verbal list, high risk medication, initial medication, final medication, error commission, error dose/frequency, error omission, error total. A generalized linear model was used to predict the time pharmacy technicians needed to obtain a MR. A log-transformed time histogram was used as the response variable for the analysis. Results were obtained after calculating the coefficients based on the maximum likelihood estimator. A Q-Q plot confirmed the appropriateness of a linear model. Variables with T-values < 2 were omitted to create a reduced model. The reduced model was plotted on a Q-Q plot and an F-test demonstrated that the reduced model was not significantly different to the full model.
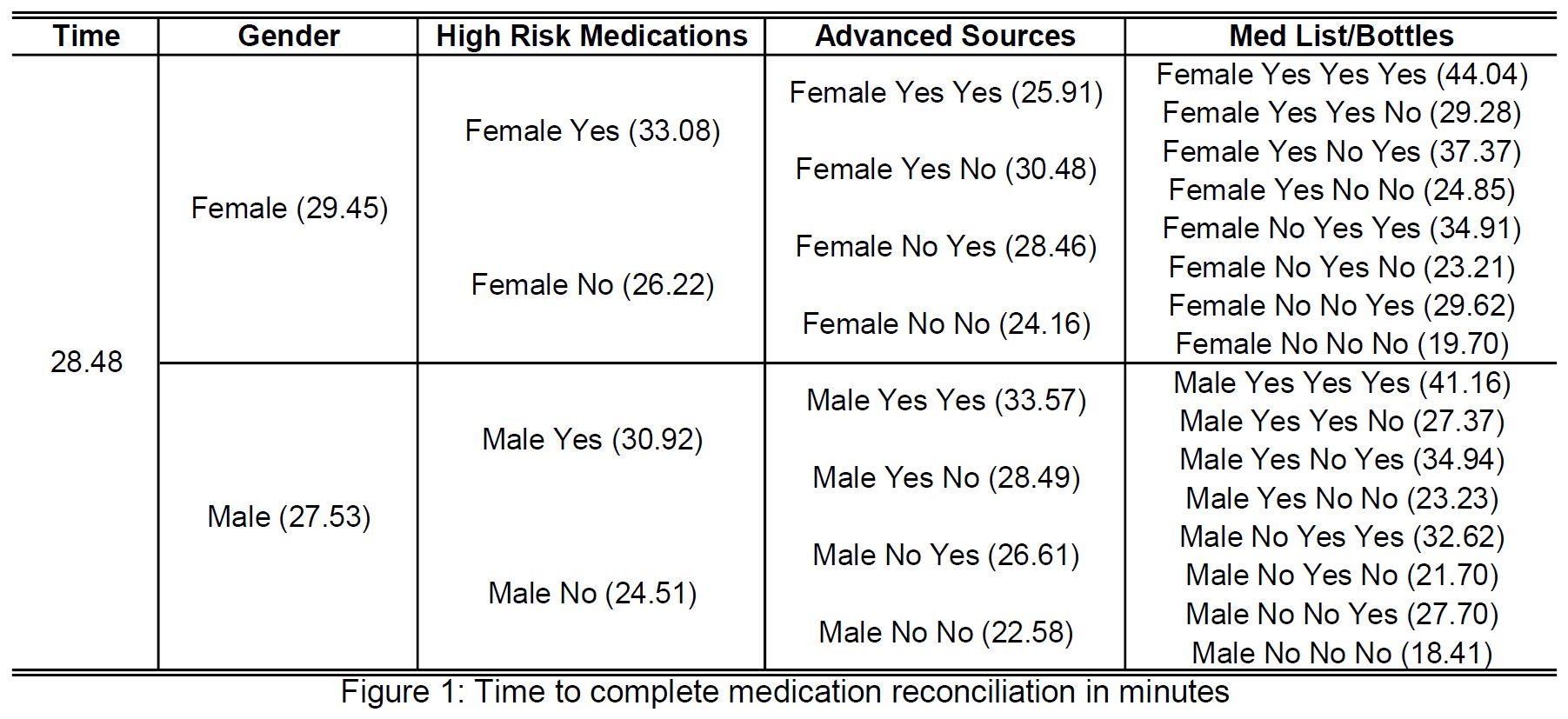
Results: The top four variables with statistically significant influence on the amount of time taken to obtain a MR include: female gender (~3.5 min longer), high risk medications (~14 min longer), advanced sources (~17 min longer), and patients with home med lists/bottles (~12 min longer) (see figure 1). It is of importance to note that each of these variables was also associated with a statistically significant increase in errors which satisfies our intuition that the more errors there are, the more effort needed to correct. Attempts were made to observe differences in ethnicity, race, and primary language but the homogeneity of our patient population did not allow for significant analysis.
Conclusions: The patient requiring the longest amount of time to obtain a MR is a female on high risk medications, utilization of advanced sources, bringing a home med list or bag full of medications. Our analysis reveals a strong cause and effect relationship between the number of errors and the time obtaining a MR. Further breakdown of the data or additional research may now be undertaken to further define relationship between error and time spent. The potential implication: training a pharmacy technician not to collect a MR from a bag full of home medications may result in reduced errors and time spent. Small modifications have been shown to produce a meaningful difference. Further analysis of the relationship between the length of time and cause of error may reveal valuable information on how to provide more efficient and cost-effective healthcare.