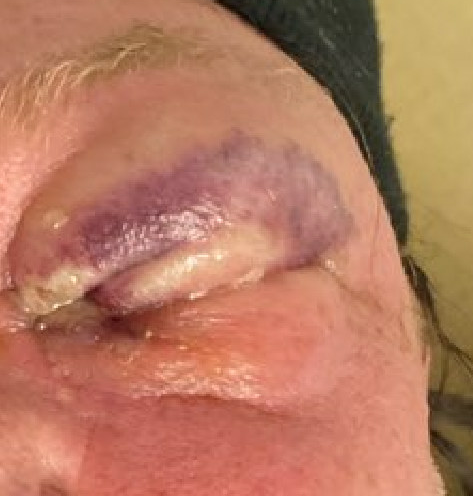
Case Presentation: The patient is a 54-year-old male with alcohol use disorder, HIV on antiretroviral therapy, and no history of diabetes, who presented with a 2-day history of painful swelling of the left upper and lower eyelids. After the first 48 hours, the patient developed purulent eye discharge and could no longer open his left eye due to swelling, which prompted him to seek medical advice. In ED, the patient reported chronic nasal discharge that he attributed to allergies. The patient denied fevers, chills, tooth pain, recent dental work, or facial trauma. BP was 100/61 HR 101Temp 37 C, RR 16 SpO2 96%. The periorbital swelling was most prominent in the left upper eyelid. It was erythematous, ecchymotic, with superficial blisters, and was moderately tender to palpation. Blood work revealed WBC 80,000 k/ul, lactate 4mmol/L, CRP 96 mg/L, ESR 92mg/L, CD4 270 /cu mm, and undetectable HIV viral load. CT orbits showed left periorbital subcutaneous soft tissue swelling suggesting preseptal cellulitis. Patient was started on vancomycin, ceftriaxone, and topical erythromycin. Despite the initial treatment, the periorbital swelling and erythema worsened over the next 24 hours, and skin overlying left periorbital area became duskier and started to slough off. Necrotizing fasciitis was strongly suspected at that time. Orbital CT was repeated, however, it only showed further progression of the soft tissue swelling without signs of gas or fascial fluid collections. Despite non-specific imaging findings, clinical suspicion for necrotizing infection remained based on rapid disease progression and signs of skin necrosis. Ophthalmology and Infectious disease teams were urgently consulted. The patient’s wound was debrided, and the diagnosis of periorbital necrotizing fasciitis was confirmed. The patient was continued on vancomycin, started on piperacillin-tazobactam, and received clindamycin for toxin suppression. Topical treatment was changed to tobramycin and mupirocin. Eventually, deep wound cultures grew penicillin-susceptible S. pyogenes and methicillin-resistant S. aureus. After 7 days of IV vancomycin and more than 20 wound debridements, the patient was discharged with a 2-week course of oral linezolid. He continued to follow up with the ophthalmology team for additional debridements prior to the complete resolution of the infection. Eventually, the patient had reconstruction surgery with skin grafting, and his vision was preserved.
Discussion: Periorbital necrotizing fasciitis is a devastating infection that carries a risk of cosmetic disfigurement, vision loss, meningitis, and death. Its early recognition is essential for proper management but presents a challenge due to its resemblance to cellulitis in its early stages. Orbital CT w/ contrast is the modality of choice for diagnosis of periorbital necrotizing fasciitis, but lacks sensitivity in diagnosing early disease as soft tissue gas may not have reached levels detectable by CT, and therefore, cannot exclude it.
Conclusions: This case emphasizes the role of clinical suspicion in the timely diagnosis of periorbital necrotizing fasciitis. No laboratory or imaging studies, alone or in combination, are sensitive or specific enough to diagnose early disease or rule it out. Early diagnosis, multidisciplinary approach, and aggressive treatment are essential and include initial broad-spectrum antibiotics, toxin suppression, and surgical debridement.