Background: Many end stage renal disease (ESRD) patients present with complaints related to missed or incomplete hemodialysis (HD). Inpatient HD units often are not credentialed for outpatient use which results in extra cost and consumes additional resources for a standard outpatient procedure. Delays in patient throughput in emergency departments (ED) can cause boarding in the ED which can lead to poor outcomes and decreased patient satisfaction. Hospital admission for missed HD can lead to longer stays than what is medically required.
Purpose: A multidisciplinary team created a unique triage pathway, Fast Track Dialysis (FTD), to improve the flow of ESRD patients presenting to the ED for missed HD.
Description: The FTD pathway rapidly identified low risk ESRD patients presenting with an urgent need for HD. FTD care was facilitated with standardized communication between Emergency Medicine (EM), Nephrology, Hospital Medicine and Nursing. The FTD pathway emphasized the option to use venous blood gases for measuring potassium levels and limited telemetry, chest X-ray, and peripheral intravenous lines when not clinically indicated.
Patients eligible for FTD were identified by EM providers. Exclusion criteria included clinical concern for illness that would require admission beyond one session of HD, arteriovenous graft or fistula issues requiring surgical or interventional radiology intervention, blood pressure greater than 200/100 mmHg, heart rate greater than 120 beats per minute, hypoxia requiring greater than 4 liters of supplemental oxygen per minute, potassium greater than 6.5 mEq/L, and the presence of concerning electrocardiogram abnormalities.
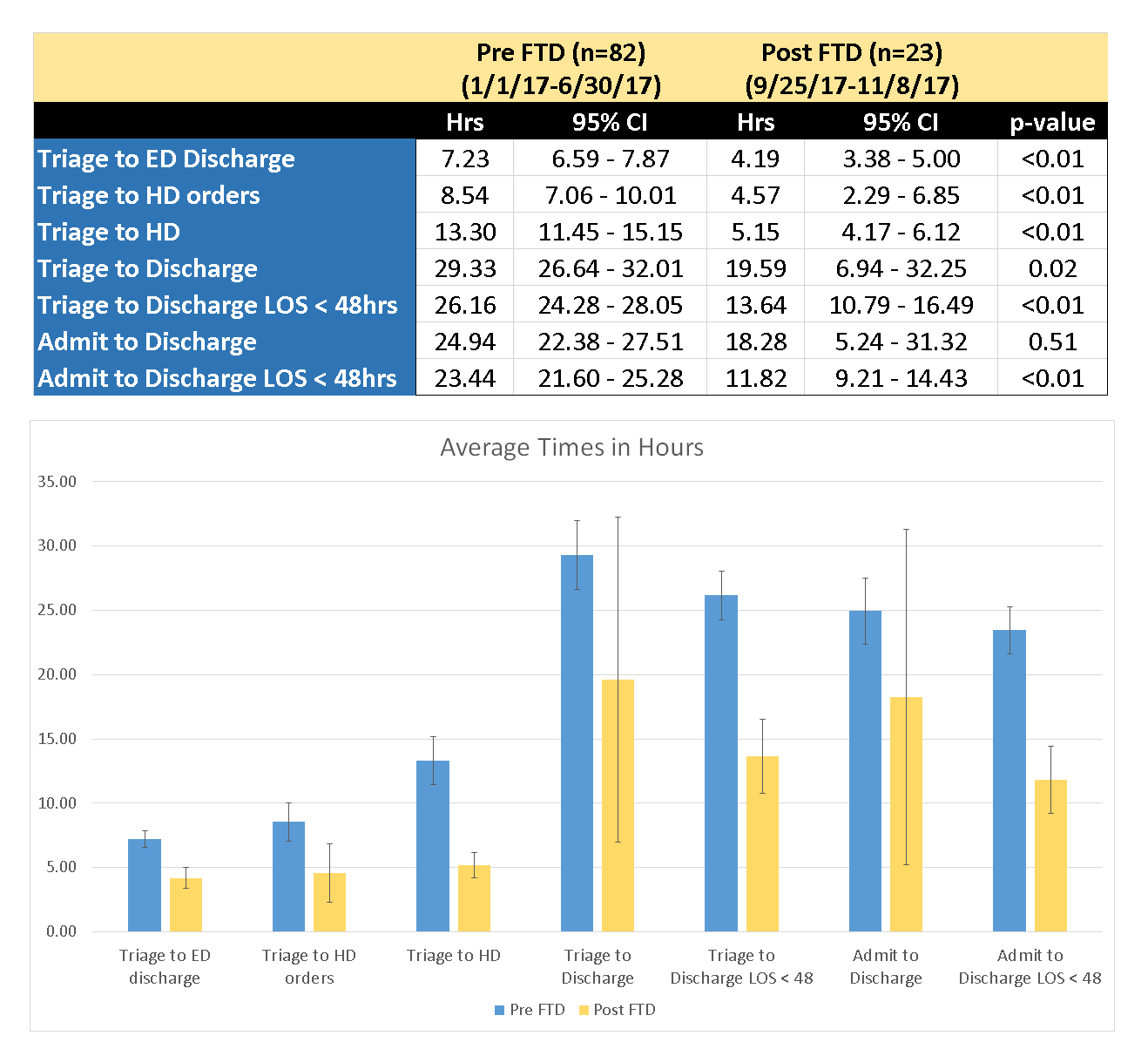
A six-month historical control group was compared with a six-week FTD cohort. The historical group was filtered by admitting diagnoses (ICD-10 codes for conditions that HD addresses and have typical length of stay of less than 48 hours) and the exclusion criteria listed above.
Conclusions: FTD led to a significant reduction in most measures studied. Time from triage to ED discharge was reduced by more than 3 hours. Time from triage to placement of HD orders decreased by nearly 4 hours. Time from triage to hospital discharge was reduced by nearly 12 hours when excluding one outlier who stayed greater than 48 hours.
The implementation of a novel patient care pathway intended to identify, triage, and facilitate the care of low risk ESRD patients who require urgent HD led to a reduction in resource utilization in an urban community and academic hospital.