Background: Not all residents pursuing an internal medicine subspecialty proceed directly to fellowship. Some trainees take one or more hospital medicine “gap years” prior to applying for fellowship. Residency program directors (PD), fellowship PDs, and faculty advisors spend substantial time advising residents on whether a gap year is the right choice for them. However, virtually no information exists regarding how frequently trainees take a gap year or how the advising process is approached. Furthermore, the decision to take a gap year is highly variable, relating to residents needing time for career decisions, opportunities for further clinical skills acquisition, crafting a more competitive application, or personal/financial reasons. Benefits and drawbacks to gap years are viewed differently by different stakeholders. Among these, only the perspectives of hospitalist leaders have been characterized, viewing short-term hires as potentially risky. There is virtually no information about how fellowship PDs approach applicants who have taken a gap year and how it influences their decision to interview and rank such applicants.
Methods: This is a qualitative study of 16 interviews among a national sample of cardiology, pulmonology/critical care medicine, hematology/oncology, and gastroenterology fellowship PDs from 5 academic institutions. Interviews were conducted in Sept-Oct 2021 and consisted of structured and semi-structured questions about perceptions of gap years. Utilizing rapid qualitative analysis, overarching themes were explored and interviews summarized. Through framework analysis, data was mapped and interpreted to describe perspectives of gap years.
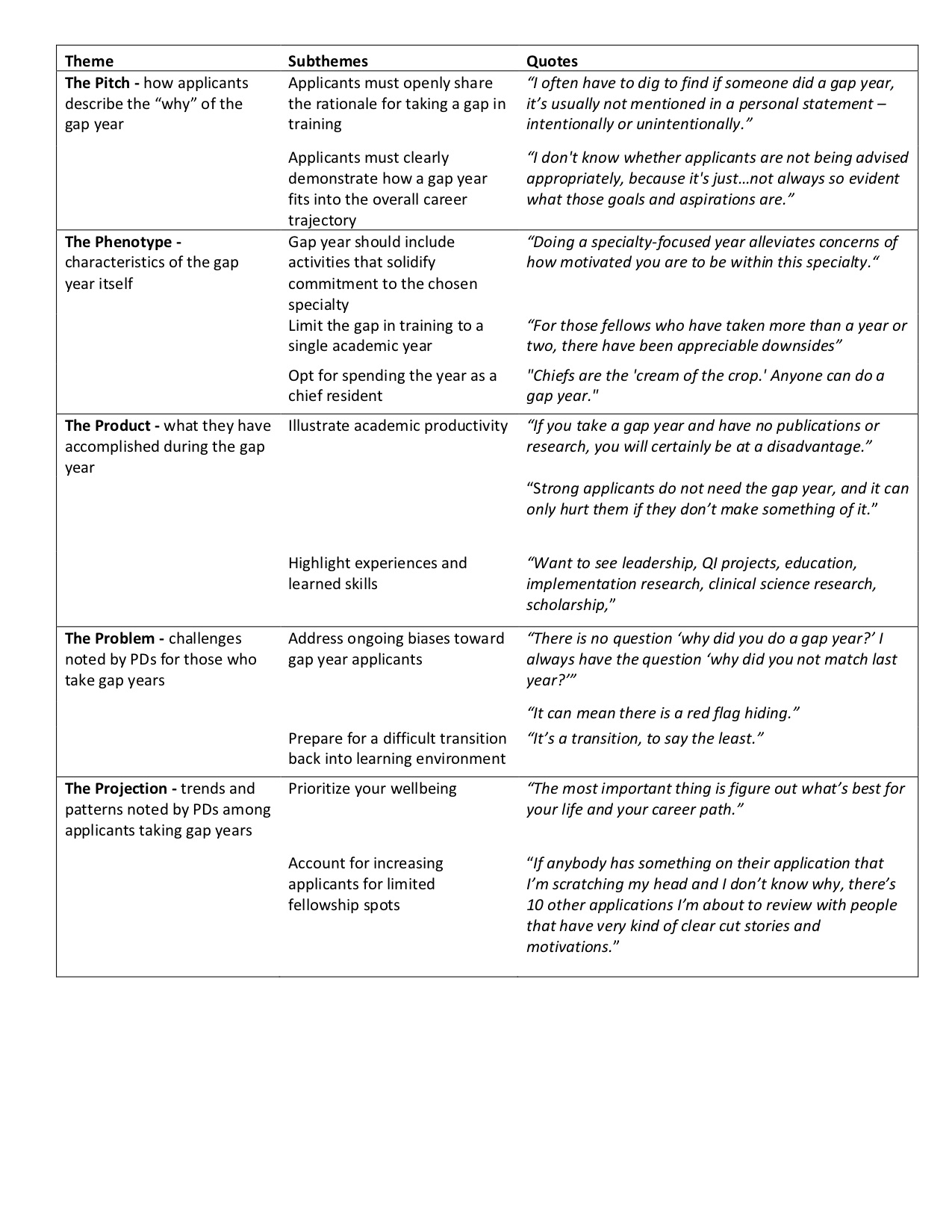
Results: Twenty fellowship PDs were approached for interviews and 16 participated. Five themes emerged: 1) explicitly state the reason for taking a gap year; 2) demonstrate ongoing commitment to the subspecialty field during the gap year; 3) specific characteristics of the gap year may positively or negatively influence perceptions of the value of that year; 4) tensions and uncertainty in evaluating applicants who have taken a gap year include fear of a hidden red flag and challenges in returning to a trainee mindset; 5) reflections on shifting trends and future projections for how gap years continue to evolve.
Conclusions: Fellowship PDs in 4 competitive internal medicine subspecialities did not view hospitalist gap years as inherently unfavorable, but placed a strong emphasis on explaining a clear and logical reason for taking a gap year, demonstrating continued commitment to the specialty, and stating how the gap year fits within the overall career trajectory. The majority of PDs stated if the reason for the gap was not readily apparent, that led to increased scrutiny of the application. Participants suggested that the personal statement offers an ideal space to summarize the gap year and craft a narrative on how the gap year makes them competitive. Participants did not universally agree on what constituted acceptable versus unacceptable reasons for taking a gap year, however, the majority agreed that “unless you have a compelling reason to take a gap year, just go ahead and apply for fellowship.” This work represents the first to explicitly describe perspectives of fellowship PDs on gap year candidates. This is a common question posed by trainees and this will help inform all who are invested in better understanding the landscape of hospital medicine gap years.