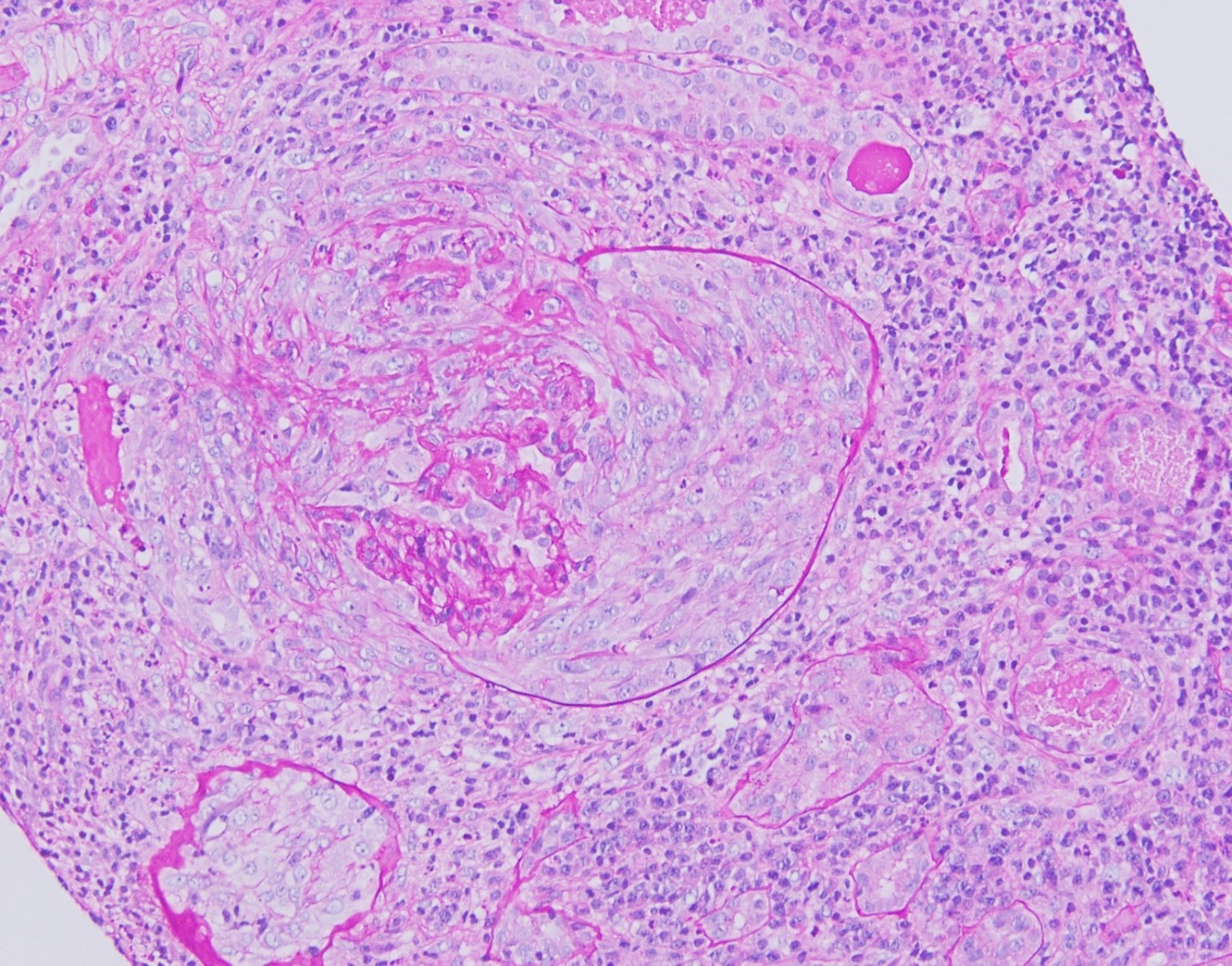
Case Presentation: A 29-year-old woman presents with fever and malaise after recently traveling abroad. Her history is notable for right ovarian cystectomy the prior year for a dermoid cyst with the postoperative course complicated by septic shock, respiratory failure requiring intubation, tracheostomy, and renal failure requiring temporary dialysis. She was eventually decannulated and her renal function mostly recovered after an extended hospital stay, and earlier this year traveled to Australia. After returning, she began having fevers, dry cough, and dyspnea. She was treated for a presumed urinary tract infection with empiric antibiotics, but her symptoms persisted and she developed poor oral intake due to vomiting. She re-presented to the emergency room and was noted to be febrile to 100.4F and tachycardic to 103. Her labs were notable for acute kidney injury with creatinine of 4.81, leukocytosis to 16.1, and urinalysis with proteinuria, hematuria, and sterile pyuria. Her CT showed left perinephric fat stranding and she was admitted for sepsis presumably due to pyelonephritis. Her fevers persisted and an extensive infectious workup, including vector borne illnesses and endemic fungi, were negative. Her renal function worsened, and her renal biopsy showed necrotizing crescent formation with linear IgG deposits consistent with anti-glomerular basement membrane (GBM) disease. The anti-GBM antibody was elevated while antineutrophil cytoplasmic antibodies (ANCA) were negative. There were no episodes of hemoptysis. She was treated with two weeks of daily plasmapheresis with albumin replacement and started on a steroid taper with cyclophosphamide. Her symptoms and renal function improved and she was discharged home. During follow up her anti-GBM antibodies and creatinine continued to downtrend.
Discussion: Anti-GBM disease is a rare disorder that typically occurs with concurrent rapidly progressive glomerulonephritis and pulmonary hemorrhage; however, it can present with isolated renal involvement as in our patient. Patients can experience nonspecific systemic symptoms of fevers, malaise, and arthralgias while labs can be notable for elevated BUN and creatinine with urinalysis showing hematuria and proteinuria. There is usually development of pathogenic anti-GBM antibodies from an inciting stimulus. Although infections have been associated as inciting stimuli, such as influenza, COVID-19, and urinary infections, there have been no reported predispositions in patients with a recent history of prior septic shock complicated by renal failure that necessitated dialysis. Our patient’s presentation of perinephric fat-stranding on CT, fevers, pyuria, and AKI lead to the initial diagnosis of pyelonephritis. Her worsening fevers and renal function despite antibiotics prompted renal biopsy that ultimately suggested anti-GBM disease.
Conclusions: Anti-GBM disease can present with nonspecific symptoms, mimicking more common conditions such as pyelonephritis as in our patient. Consider autoimmune processes in patients with worsening renal function despite appropriate empiric treatment. There should be a low threshold to obtain a kidney biopsy if anti-GBM is suspected as a delay in diagnosis can lead to irreversible kidney failure.